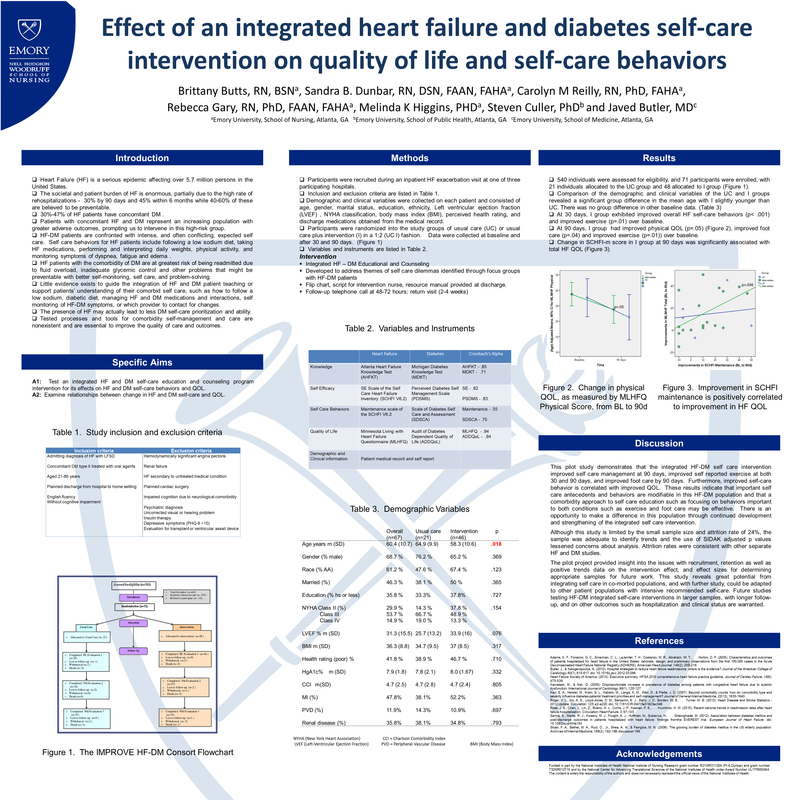
-
Butts Research
- Meet the Team
- Metabolomic Pathways of Symptoms in Black Adults with Heart Failure
- Skeletal Muscle in Heart Failure with Preserved Ejection Fraction
- Inflammasome in Heart Failure
- Exercise and Heart Failure
- Telomeres in Heart Failure
- Heart Failure Research Studies
- Publications
- Presentation Abstracts
- Atlanta Heart Failure Knowledge Test
- PREVAIL Lab
- MVP Study
- CARDI Study
- Past Studies
- Pathophysiology Videos
- Genetics Workshop (UNC)
- Omics Workshop (SNRS 2023)
- Diabetes Prevention and Insulin
- AHFKT
2022 Presentations
Two Year Cognitive and Biomarker Change in a Racially Diverse, Middle-aged, Cohort at Risk for Alzheimer’s Disease
Alzheimer's Association International Conference 2022, San Diego, CA
2021 Presentations
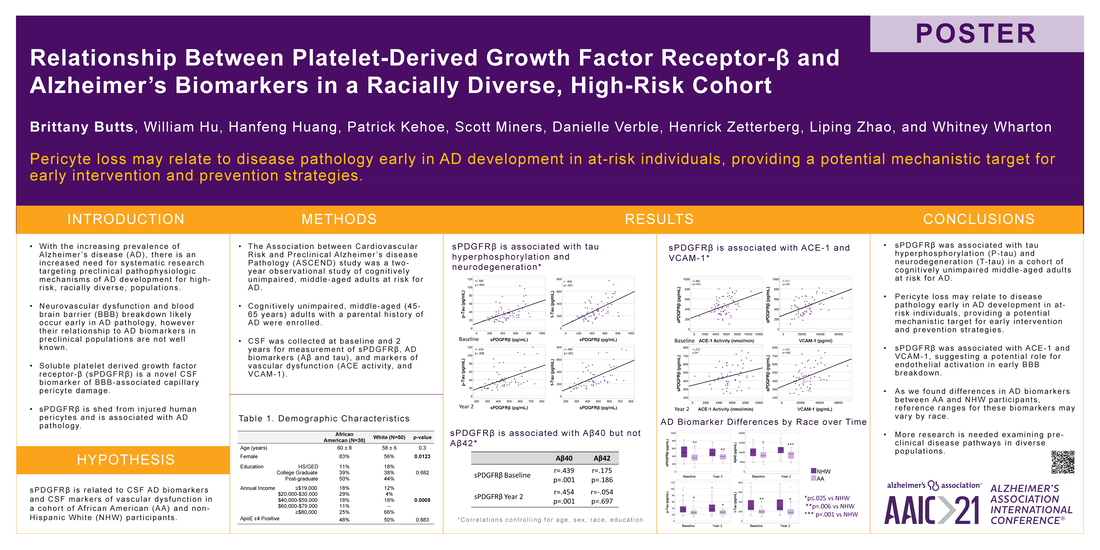
Relationship Between Platelet-Derived Growth Factor Receptor‐β and Alzheimer’s Biomarkers in a Racially Diverse, High-Risk Cohort
Alzheimer's Association International Conference 2021, Denver, CO
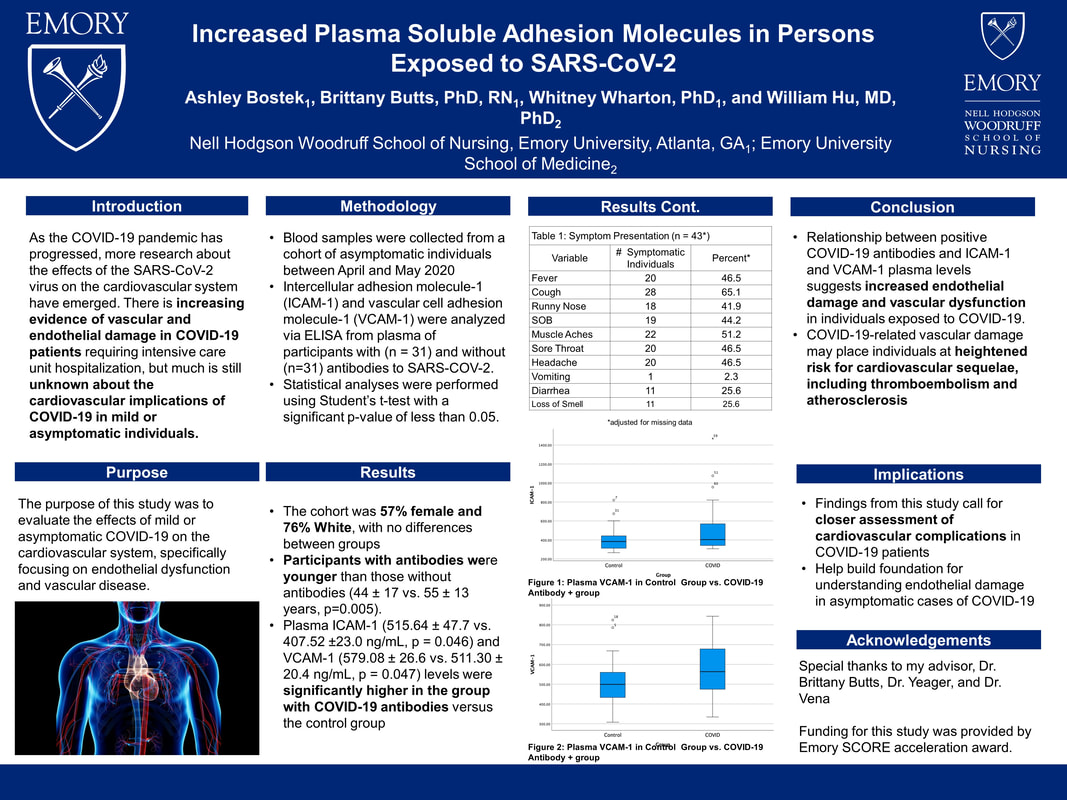
Increased Plasma Soluble Adhesion Molecules in Persons Exposed to SARS-CoV-2
Developing a Remote Clinical Research Protocol: Lessons Learned in the Age of COVID-19
2020 Presentations
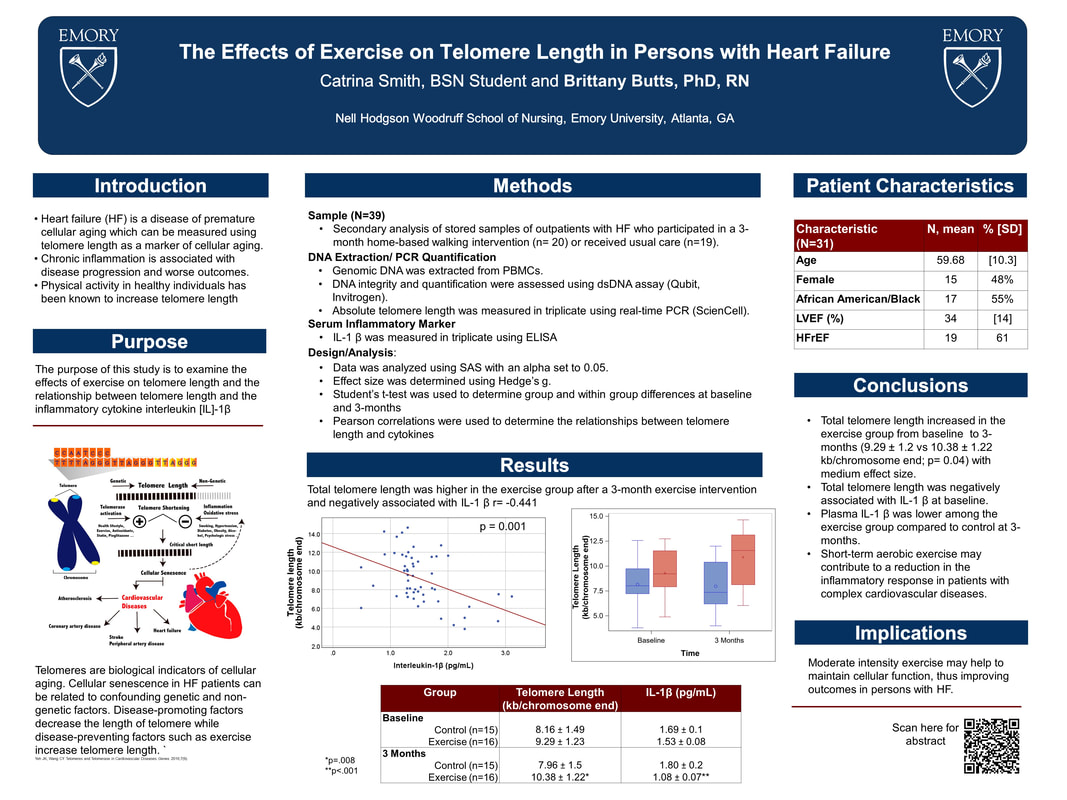
Effects of Exercise on Telomere Length in Persons with Heart Failure
2019 Presentations
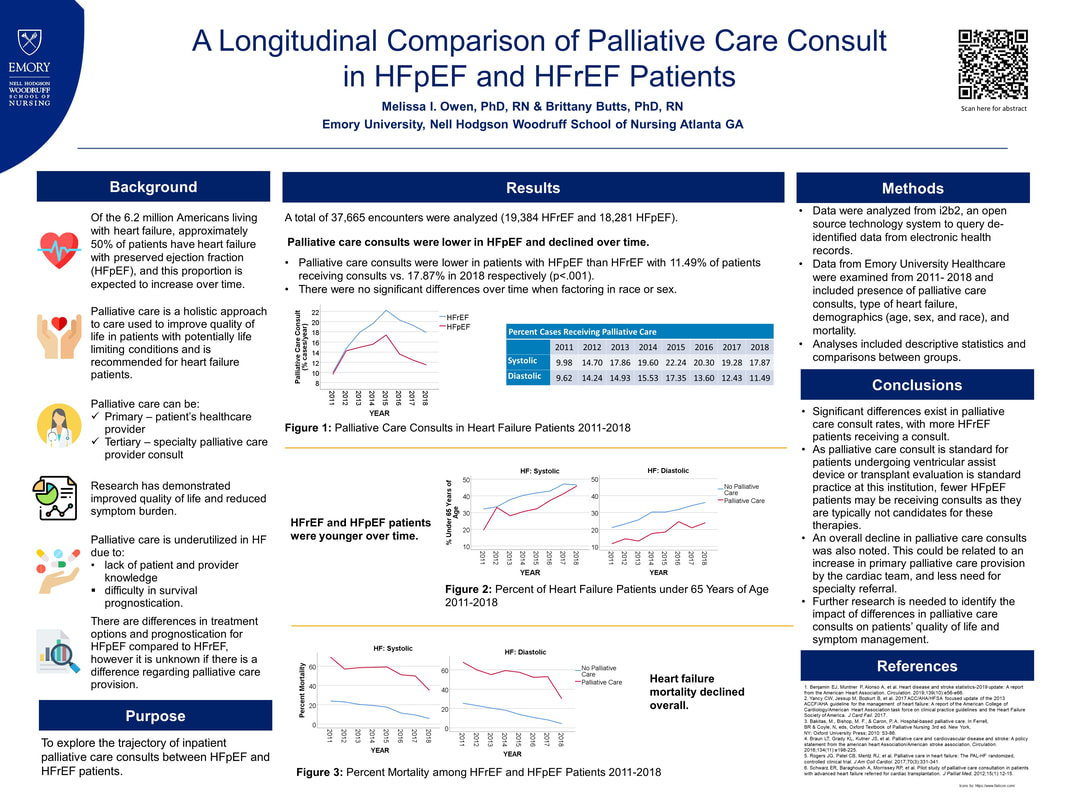
A Longitudinal Comparison of Palliative Care Consult in HFpEF and HFrEF Patients
2018 Conference Presentations
|
American Heart Association Scientific Sessions, Chicago, IL, November 2018
|
Pericardial Fluid Chymase Activity Four Hours Post Cardiac Surgery is Related to Intensive Care Unit and Total Hospital Length of Stay
Introduction: Operative trauma, reperfusion injury, and other insults from cardiac surgery lead to a robust cardiac inflammatory response and have a significant impact on post-surgical outcomes and hospital utilization. Chymase activity and inflammatory cytokines are elevated in pericardial fluid (PCF) as early as 4 hours post surgery and are many-fold higher than in blood. The post-surgical pericardial environment may provide more insight into risk of adverse postoperative outcomes.
Objective: To examine associations between key biomarkers of cardiac injury and inflammation in the PCF 4 hours after cardiac surgery with intensive care unit (ICU) and total hospital length of stay.
Methods: PCF was collected from adult patients (N=30) 4 hours post cardiac surgery in this exploratory retrospective study. Radiolabeled (125I) angiotensin-1-12 was used as a substrate for the determination of chymase activity. PCF biomarkers were measured using a Luminex bead based multiplex assay. ICU and total length of stay was determined from the medical record. Zero-truncated poisson regression models were used to model length of stay.
Results: Mean ICU stay was 2.17 ± 3.8 days and mean total length of stay was 6.41 ± 1.3 days. Univariate analysis demonstrated that the Society of Thoracic Surgeons Predicted Risk of Morbidity and Mortality Score (STS-PROM) and 4-hour PCF chymase activity, and CXCL6 were independent predictors of both ICU and total hospital length of stay. Multivariable models including STS-PROM as a predictor demonstrated that 4-hour PCF chymase activity had the best fit model for both ICU and total length of stay.
Conclusions: This exploratory study found that mast cell and neutrophil inflammatory markers in PCF 4 hours after cardiac surgery were related to both ICU and total hospital length of stay. Chymase activity had the best fit relationship with length of stay, suggesting 4-hour chymase activity may improve prediction of patient ICU utilization after cardiac surgery. Postoperative pericardial drainage may be a potential tool for predicting outcomes after cardiac surgery. A more accurate prediction of post-operative outcomes would benefit individual patients for better management of care and for organizations to optimize resource utilization.
Introduction: Operative trauma, reperfusion injury, and other insults from cardiac surgery lead to a robust cardiac inflammatory response and have a significant impact on post-surgical outcomes and hospital utilization. Chymase activity and inflammatory cytokines are elevated in pericardial fluid (PCF) as early as 4 hours post surgery and are many-fold higher than in blood. The post-surgical pericardial environment may provide more insight into risk of adverse postoperative outcomes.
Objective: To examine associations between key biomarkers of cardiac injury and inflammation in the PCF 4 hours after cardiac surgery with intensive care unit (ICU) and total hospital length of stay.
Methods: PCF was collected from adult patients (N=30) 4 hours post cardiac surgery in this exploratory retrospective study. Radiolabeled (125I) angiotensin-1-12 was used as a substrate for the determination of chymase activity. PCF biomarkers were measured using a Luminex bead based multiplex assay. ICU and total length of stay was determined from the medical record. Zero-truncated poisson regression models were used to model length of stay.
Results: Mean ICU stay was 2.17 ± 3.8 days and mean total length of stay was 6.41 ± 1.3 days. Univariate analysis demonstrated that the Society of Thoracic Surgeons Predicted Risk of Morbidity and Mortality Score (STS-PROM) and 4-hour PCF chymase activity, and CXCL6 were independent predictors of both ICU and total hospital length of stay. Multivariable models including STS-PROM as a predictor demonstrated that 4-hour PCF chymase activity had the best fit model for both ICU and total length of stay.
Conclusions: This exploratory study found that mast cell and neutrophil inflammatory markers in PCF 4 hours after cardiac surgery were related to both ICU and total hospital length of stay. Chymase activity had the best fit relationship with length of stay, suggesting 4-hour chymase activity may improve prediction of patient ICU utilization after cardiac surgery. Postoperative pericardial drainage may be a potential tool for predicting outcomes after cardiac surgery. A more accurate prediction of post-operative outcomes would benefit individual patients for better management of care and for organizations to optimize resource utilization.
|
American College of Cardiology Scientific Sessions, Orlando, FL, March 2018
|
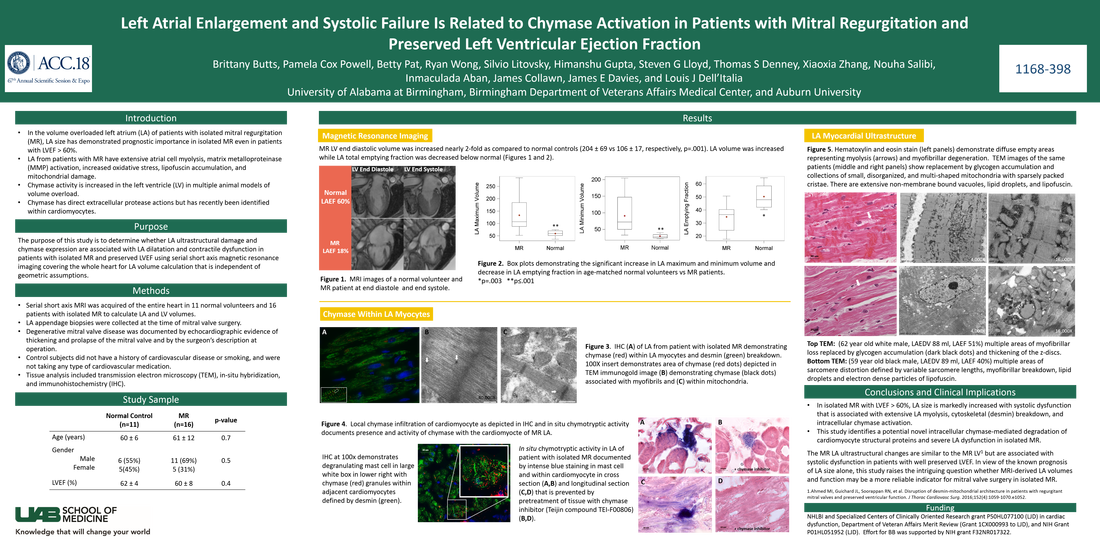
Left Atrial Enlargement and Systolic Failure is Related to Chymase Activation in Patients with Mitral Regurgitation and Preserved Left Ventricular Ejection Fraction
Background: Left ventricular ejection fraction (LVEF) is spuriously elevated and is an unreliable predictor of outcome after surgery for mitral regurgitation (MR). Chymase activity is increased in the left ventricle (LV) in multiple animal models of a pure volume overload (VO). Chymase has direct protease actions that activate MMPs and degrade extracellular matrix proteins. Left atrial (LA) size is an independent predictor of outcome in patients with isolated MR, but LA function and remodeling is unknown. Here we test the hypothesis that chymase expression is related to the severity of VO in the LA and LV of patients with isolated MR and LVEF > 60%.
Methods: Serial short axis MRI was acquired of the entire heart in 10 normal volunteers and 16 patients with isolated MR to calculate LA and LV volumes. LA appendage biopsies were collected at the time of mitral valve surgery and from normal hearts rejected for transplant.
Results: MR LVEDV was increased nearly 2-fold, and LVEF did not differ from normal. LA volume was increased 3-fold, while LAEF was 50% below normal. As in previous studies of the MR LV, transmission electron microscopy (TEM) of the LA appendage demonstrated mitochondrial disarray, blurring of z disc, myofibrillar breakdown, and electron dense accumulations consistent with lipofuscin. Immunohistochemistry (IHC) demonstrates chymase within LA myocytes and TEM immunogold localizes chymase in the z disc and myofibrils and within mitochondria. Analysis of pericardial fluid demonstrates chymase in exosomes, and mass spectrometry demonstrates abundant serine protease inhibitors α2 macroglobulin and α1 anti-chymotrypsin. Preliminary data suggest LA chymase activity is increased 10-fold in the MR LA vs. normal. In situ chymotryptic tissue assay demonstrated proteolytic presence of chymase in LA myocytes with IHC evidence of desmin, myosin, and connexin 43 breakdown.
Conclusion. In isolated MR with LVEF > 60%, LA size is markedly increased with severe dysfunction and is related to the extent of chymase activation. This study identifies a potential novel intracellular chymase-mediated degradation of cardiomyocyte structural proteins and severe LA dysfunction in isolated MR.
Background: Left ventricular ejection fraction (LVEF) is spuriously elevated and is an unreliable predictor of outcome after surgery for mitral regurgitation (MR). Chymase activity is increased in the left ventricle (LV) in multiple animal models of a pure volume overload (VO). Chymase has direct protease actions that activate MMPs and degrade extracellular matrix proteins. Left atrial (LA) size is an independent predictor of outcome in patients with isolated MR, but LA function and remodeling is unknown. Here we test the hypothesis that chymase expression is related to the severity of VO in the LA and LV of patients with isolated MR and LVEF > 60%.
Methods: Serial short axis MRI was acquired of the entire heart in 10 normal volunteers and 16 patients with isolated MR to calculate LA and LV volumes. LA appendage biopsies were collected at the time of mitral valve surgery and from normal hearts rejected for transplant.
Results: MR LVEDV was increased nearly 2-fold, and LVEF did not differ from normal. LA volume was increased 3-fold, while LAEF was 50% below normal. As in previous studies of the MR LV, transmission electron microscopy (TEM) of the LA appendage demonstrated mitochondrial disarray, blurring of z disc, myofibrillar breakdown, and electron dense accumulations consistent with lipofuscin. Immunohistochemistry (IHC) demonstrates chymase within LA myocytes and TEM immunogold localizes chymase in the z disc and myofibrils and within mitochondria. Analysis of pericardial fluid demonstrates chymase in exosomes, and mass spectrometry demonstrates abundant serine protease inhibitors α2 macroglobulin and α1 anti-chymotrypsin. Preliminary data suggest LA chymase activity is increased 10-fold in the MR LA vs. normal. In situ chymotryptic tissue assay demonstrated proteolytic presence of chymase in LA myocytes with IHC evidence of desmin, myosin, and connexin 43 breakdown.
Conclusion. In isolated MR with LVEF > 60%, LA size is markedly increased with severe dysfunction and is related to the extent of chymase activation. This study identifies a potential novel intracellular chymase-mediated degradation of cardiomyocyte structural proteins and severe LA dysfunction in isolated MR.
2017 Conference Presentations
Oxidative Stress is Related to Increased Sodium-Aldosterone Product and Left Ventricular Dysfunction in Resistant Hypertension
Introduction: Resistant hypertension (R-HTN) is associated with hyperaldosteronism that responds to either salt restriction or aldosterone receptor blockade. Endothelial dysfunction is an important risk factor in hypertensive cardiovascular disease. The extrarenal effects of aldosterone on vascular cells are exacerbated by increased dietary sodium. We hypothesized that increased xanthine oxidase (XO), a product of endothelial cells, is related to expression of renin-angiotensin system and aldosterone-salt product and to left ventricular (LV) function in R-HTN.
Methods: Persons with R-HTN (n=91) on ≥ 4 medications with blood pressure > 140/90 mmHg and non-resistant hypertension (NR-HTN, n=25) had blood collected for aldosterone level and XO and renin activities; 24-hour urine collected for sodium, aldosterone and renin; and cardiac MRI performed to measure LV function and morphology. 67 normal subjects on no cardiovascular medications served as controls for XO analysis, which was determined by HPLC. A subset of R-HTN (n=19) received spironolactone without salt restriction for 6 months with follow-up XO and MRI measures.
Results and Conclusions: XO activity was greater in R-HTN vs NR-HTN (2.98 ±0.4 vs 1.87±0.4 µU/ml, p=.02) and was increased in both hypertensive groups when compared with controls (1.68 ± 0.4 µU/ml). Diastolic dysfunction (e’, p=.03) and increased LV end-diastolic mass (EDM, p<.001), volume (EDV, p=.03), and wall thickness (p=.006) were present in R-HTN but not NR-HTN. Among R-HTN, XO activity was positively correlated with increased LV EDM (rho=.201, p=.03), LV EDV (rho=.217, p=.02), 24-hour urine sodium-aldosterone product (rho=.256, p=.008), and serum aldosterone-renin ratio (rho=.252, p=.007) and negatively correlated with 24-hour urinary renin activity (rho=-.206, p=.03). No relationships with XO activity among these parameters in NR-HTN were found. In the subset of R-HTN receiving spironolactone without salt restriction, LV mass decreased but LV diastolic function and XO activity did not improve by 6 months. These results demonstrated a potential role of endothelium-derived oxidative stress and salt in the pathophysiology of R-HTN and diastolic dysfunction that did not reverse by the addition of spironolactone.
Introduction: Resistant hypertension (R-HTN) is associated with hyperaldosteronism that responds to either salt restriction or aldosterone receptor blockade. Endothelial dysfunction is an important risk factor in hypertensive cardiovascular disease. The extrarenal effects of aldosterone on vascular cells are exacerbated by increased dietary sodium. We hypothesized that increased xanthine oxidase (XO), a product of endothelial cells, is related to expression of renin-angiotensin system and aldosterone-salt product and to left ventricular (LV) function in R-HTN.
Methods: Persons with R-HTN (n=91) on ≥ 4 medications with blood pressure > 140/90 mmHg and non-resistant hypertension (NR-HTN, n=25) had blood collected for aldosterone level and XO and renin activities; 24-hour urine collected for sodium, aldosterone and renin; and cardiac MRI performed to measure LV function and morphology. 67 normal subjects on no cardiovascular medications served as controls for XO analysis, which was determined by HPLC. A subset of R-HTN (n=19) received spironolactone without salt restriction for 6 months with follow-up XO and MRI measures.
Results and Conclusions: XO activity was greater in R-HTN vs NR-HTN (2.98 ±0.4 vs 1.87±0.4 µU/ml, p=.02) and was increased in both hypertensive groups when compared with controls (1.68 ± 0.4 µU/ml). Diastolic dysfunction (e’, p=.03) and increased LV end-diastolic mass (EDM, p<.001), volume (EDV, p=.03), and wall thickness (p=.006) were present in R-HTN but not NR-HTN. Among R-HTN, XO activity was positively correlated with increased LV EDM (rho=.201, p=.03), LV EDV (rho=.217, p=.02), 24-hour urine sodium-aldosterone product (rho=.256, p=.008), and serum aldosterone-renin ratio (rho=.252, p=.007) and negatively correlated with 24-hour urinary renin activity (rho=-.206, p=.03). No relationships with XO activity among these parameters in NR-HTN were found. In the subset of R-HTN receiving spironolactone without salt restriction, LV mass decreased but LV diastolic function and XO activity did not improve by 6 months. These results demonstrated a potential role of endothelium-derived oxidative stress and salt in the pathophysiology of R-HTN and diastolic dysfunction that did not reverse by the addition of spironolactone.
American Heart Association Scientific Sessions, Anaheim, CA, November 2017
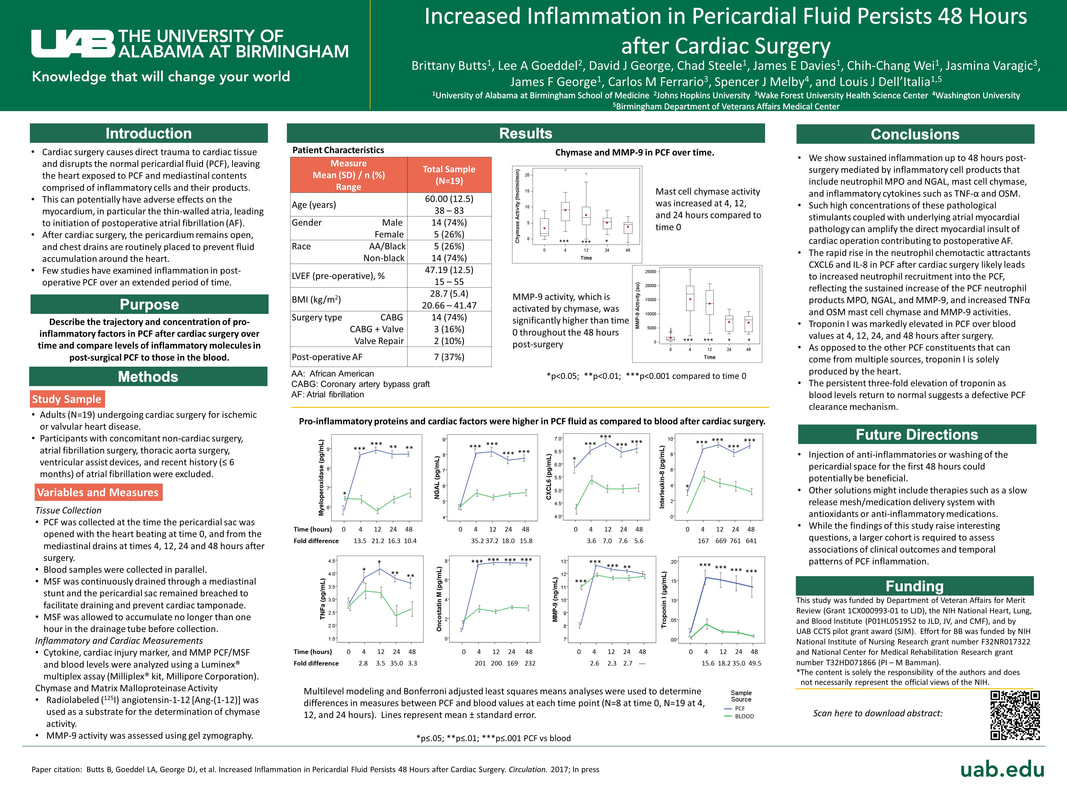
Increased Inflammation in Pericardial Fluid Persists 48 Hours After Cardiac Surgery
Introduction: Cardiac surgery causes direct trauma to cardiac tissue and disrupts the normal pericardial fluid (PCF), leaving the heart exposed to PCF and mediastinal contents comprised of inflammatory cells and their products. This can potentially have adverse effects on the myocardium, in particular the thin-walled atria, leading to initiation of postoperative atrial fibrillation (AF). After cardiac surgery, the pericardium remains open, and chest drains are routinely placed to prevent fluid accumulation around the heart. However, few studies have examined inflammation in post-operative PCF composition over an extended period of time.
Purpose: The purpose of this study is to describe the trajectory and concentration of pro-inflammatory factors in PCF after cardiac surgery over time and compare levels of inflammatory molecules in post-surgical PCF to those in the blood.
Methods: PCF was collected immediately after the pericardial sac was incised with the heart beating (time 0), and from the mediastinal drains at times 4, 12, 24 and 48 hours after surgery in adults (N=18) undergoing cardiac surgery for ischemic or valvular heart disease. Blood samples were collected in parallel. Paired t-tests were used to determine differences in measures between PCF and blood values at each time point.
Results and Conclusions: Neutrophil (MPO, NGAL, CXCL6, and IL-8) and cardiac inflammatory (TNFα and OSM) factors were 4- to 700-fold higher in PCF compared to blood over the 4 to 48 hour time course. PCF mast cell chymase activity was increased through 24 hours compared to time 0; while MMP-9 activity, activated by chymase, was significantly higher than time 0 through 48 hours. There was a persistent 3-fold elevation of troponin-1 through 48 hours, suggesting a defective PCF clearance mechanism rather than direct drainage. Multiple circulating inflammatory factors have been linked to atrial remodeling and AF in multiple studies. The highly inflammatory post-operative PCF that can only be cleared by suction leads us to speculate that early drain removal may be a cause for postoperative cardiac complications, in particular post-operative atrial fibrillation. Future research examining outcomes related to PCF inflammation and AF risk is warranted.
Increased Inflammation in Pericardial Fluid Persists 48 Hours After Cardiac Surgery
Introduction: Cardiac surgery causes direct trauma to cardiac tissue and disrupts the normal pericardial fluid (PCF), leaving the heart exposed to PCF and mediastinal contents comprised of inflammatory cells and their products. This can potentially have adverse effects on the myocardium, in particular the thin-walled atria, leading to initiation of postoperative atrial fibrillation (AF). After cardiac surgery, the pericardium remains open, and chest drains are routinely placed to prevent fluid accumulation around the heart. However, few studies have examined inflammation in post-operative PCF composition over an extended period of time.
Purpose: The purpose of this study is to describe the trajectory and concentration of pro-inflammatory factors in PCF after cardiac surgery over time and compare levels of inflammatory molecules in post-surgical PCF to those in the blood.
Methods: PCF was collected immediately after the pericardial sac was incised with the heart beating (time 0), and from the mediastinal drains at times 4, 12, 24 and 48 hours after surgery in adults (N=18) undergoing cardiac surgery for ischemic or valvular heart disease. Blood samples were collected in parallel. Paired t-tests were used to determine differences in measures between PCF and blood values at each time point.
Results and Conclusions: Neutrophil (MPO, NGAL, CXCL6, and IL-8) and cardiac inflammatory (TNFα and OSM) factors were 4- to 700-fold higher in PCF compared to blood over the 4 to 48 hour time course. PCF mast cell chymase activity was increased through 24 hours compared to time 0; while MMP-9 activity, activated by chymase, was significantly higher than time 0 through 48 hours. There was a persistent 3-fold elevation of troponin-1 through 48 hours, suggesting a defective PCF clearance mechanism rather than direct drainage. Multiple circulating inflammatory factors have been linked to atrial remodeling and AF in multiple studies. The highly inflammatory post-operative PCF that can only be cleared by suction leads us to speculate that early drain removal may be a cause for postoperative cardiac complications, in particular post-operative atrial fibrillation. Future research examining outcomes related to PCF inflammation and AF risk is warranted.
Southern Nursing Research Society, February 2017, Dallas, TX
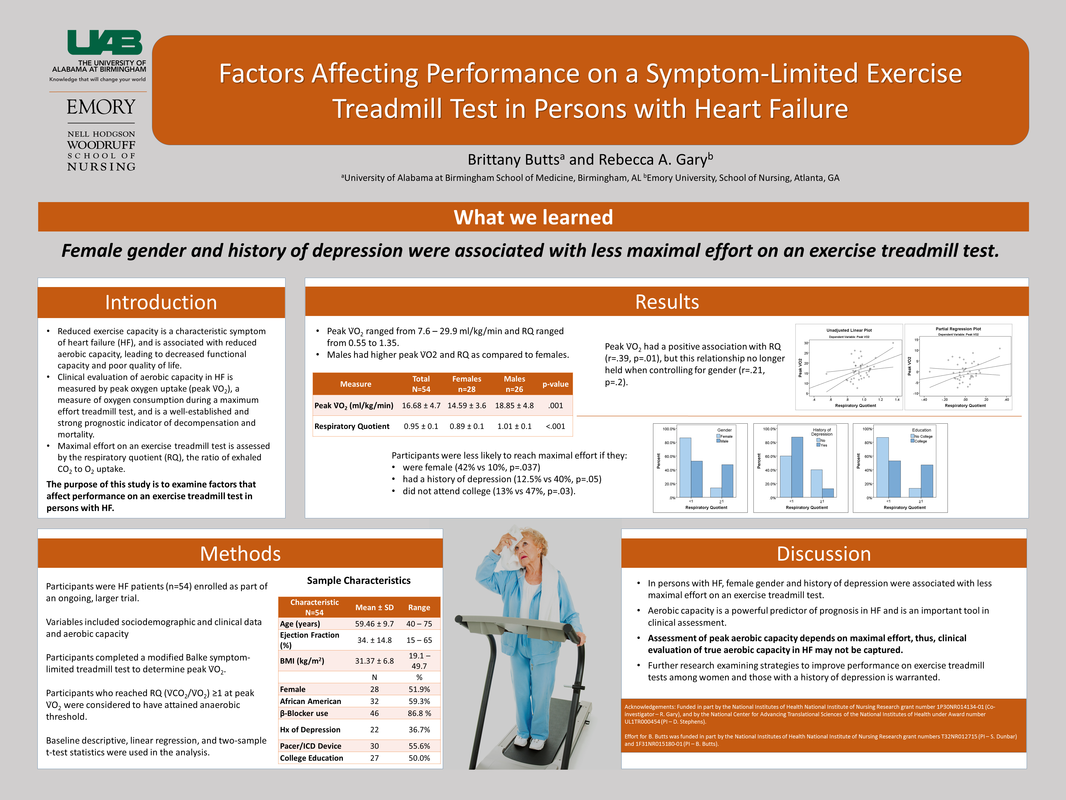
Factors Affecting Performance on a Symptom-Limited Exercise Treadmill Test in Persons with Heart Failure
Brittany Butts and Rebecca Gary
Introduction: Reduced exercise capacity is a characteristic symptom of heart failure (HF), and is associated with reduced aerobic capacity, leading to decreased functional capacity and poor quality of life. Clinical evaluation of aerobic capacity in HF is measured by peak oxygen uptake (peak V̇O2), a measure of oxygen consumption during a maximum effort treadmill test, and is a well-established and strong prognostic indicator of decompensation and mortality. Maximal effort on an exercise treadmill test is assessed by the respiratory quotient (RQ), the ratio of exhaled CO2 to O2 uptake. The purpose of this study is to examine factors that affect performance on an exercise treadmill test in persons with HF.
Methods: Persons with HF (N=41) completed a modified Balke symptom-limited treadmill test to determine peak V̇O2. Sociodemographic and clinical variables included age, gender, race, and medical history, and were obtained from a self-report questionnaire. Participants who reached RQ (V̇CO2/V̇O2) ≥1 at peak V̇O2 were considered to have attained anaerobic threshold.
Results: Peak V̇O2 ranged from 7.6 – 29.9 ml/kg/min. Males had higher peak V̇O2 as compared to females (18.85 ± 4.8 vs 14.59 ± 3.6 ml/kg/min, p=.001). In addition, males had higher RQ than females (1.01 ± 0.1 vs 0.89 ± 0.1, p<.001), and a higher proportion of males met anaerobic threshold than females (42% vs 10%, p=.037). Participants were less likely to reach maximal effort if they had a history of depression (12.5% vs 40%, p=.05) and did not attend college (13% vs 47%, p=.03). Peak V̇O2 had a positive association with RQ (r=.39, p=.01), but this relationship no longer held when controlling for gender (r=.21, p=.2).
Conclusions: In persons with HF, female gender and history of depression were associated with less maximal effort on an exercise treadmill test. Aerobic capacity is a powerful predictor of prognosis in HF and is an important tool in clinical assessment. Assessment of peak aerobic capacity depends on maximal effort, thus, clinical evaluation of true aerobic capacity in HF may not be captured. Further research examining strategies to improve performance on exercise treadmill tests among women and those with a history of depression is warranted.
Factors Affecting Performance on a Symptom-Limited Exercise Treadmill Test in Persons with Heart Failure
Brittany Butts and Rebecca Gary
Introduction: Reduced exercise capacity is a characteristic symptom of heart failure (HF), and is associated with reduced aerobic capacity, leading to decreased functional capacity and poor quality of life. Clinical evaluation of aerobic capacity in HF is measured by peak oxygen uptake (peak V̇O2), a measure of oxygen consumption during a maximum effort treadmill test, and is a well-established and strong prognostic indicator of decompensation and mortality. Maximal effort on an exercise treadmill test is assessed by the respiratory quotient (RQ), the ratio of exhaled CO2 to O2 uptake. The purpose of this study is to examine factors that affect performance on an exercise treadmill test in persons with HF.
Methods: Persons with HF (N=41) completed a modified Balke symptom-limited treadmill test to determine peak V̇O2. Sociodemographic and clinical variables included age, gender, race, and medical history, and were obtained from a self-report questionnaire. Participants who reached RQ (V̇CO2/V̇O2) ≥1 at peak V̇O2 were considered to have attained anaerobic threshold.
Results: Peak V̇O2 ranged from 7.6 – 29.9 ml/kg/min. Males had higher peak V̇O2 as compared to females (18.85 ± 4.8 vs 14.59 ± 3.6 ml/kg/min, p=.001). In addition, males had higher RQ than females (1.01 ± 0.1 vs 0.89 ± 0.1, p<.001), and a higher proportion of males met anaerobic threshold than females (42% vs 10%, p=.037). Participants were less likely to reach maximal effort if they had a history of depression (12.5% vs 40%, p=.05) and did not attend college (13% vs 47%, p=.03). Peak V̇O2 had a positive association with RQ (r=.39, p=.01), but this relationship no longer held when controlling for gender (r=.21, p=.2).
Conclusions: In persons with HF, female gender and history of depression were associated with less maximal effort on an exercise treadmill test. Aerobic capacity is a powerful predictor of prognosis in HF and is an important tool in clinical assessment. Assessment of peak aerobic capacity depends on maximal effort, thus, clinical evaluation of true aerobic capacity in HF may not be captured. Further research examining strategies to improve performance on exercise treadmill tests among women and those with a history of depression is warranted.
2016 Conference Presentations
Oral Abstract Presentation
Background: Aerobic capacity, as measured by peak oxygen uptake (V̇O2), is one of the most powerful predictors of prognosis in heart failure (HF). Inflammation is a key factor contributing to alterations in aerobic capacity, and the interleukin (IL)-1 cytokine IL-1β is implicated in this process. The adaptor protein ASC (apoptosis associated speck-like protein containing a caspase recruitment domain) is necessary for inflammasome activation of IL-1β. ASC expression is controlled through epigenetic modification, and lower ASC methylation is associated with worse outcomes in HF.
Hypothesis: Peak V̇O2 will be positively related to ASC methylation and negatively related to IL-1β in persons with HF.
Methods: This cross-sectional study examined the relationship between ASC methylation and the inflammatory cytokine IL-1β with peak V̇O2 in 54 stable outpatients with HF. All participants were NYHA class II or III, not currently engaged in an exercise program, and physically able to complete a symptom limited modified Balke exercise treadmill test.
Results: Participants were 59 ± 10 years of age, 52% female, and 59% African American. Mean peak V̇O2 was 16.68 ± 4.7 ml/kg/min. Peak V̇O2 was positively associated with mean percent ASC methylation (r=.47, p=.001) and negatively associated with IL-1β (r=-.38, p=.007). Multiple linear regression models controlling for left ventricular ejection fraction and gender demonstrated that peak V̇O2 increased by 2.30 ml/kg/min for every 1% increase in mean ASC methylation and decreased by 1.91 ml/kg/min for every 1 pg/mL increase in plasma IL-1β.
Conclusions: Mean percent ASC methylation and plasma IL-1β levels are associated with clinically meaningful changes in peak V̇O2 in persons with HF. Inflammasome activation may play a mechanistic role in determining aerobic capacity. ASC methylation is a potentially modifiable mechanism for reducing the inflammatory response, thereby improving aerobic capacity in HF. Modification of ASC expression via behavioral interventions that increase ASC methylation, may improve aerobic capacity in persons with HF.
Background: Aerobic capacity, as measured by peak oxygen uptake (V̇O2), is one of the most powerful predictors of prognosis in heart failure (HF). Inflammation is a key factor contributing to alterations in aerobic capacity, and the interleukin (IL)-1 cytokine IL-1β is implicated in this process. The adaptor protein ASC (apoptosis associated speck-like protein containing a caspase recruitment domain) is necessary for inflammasome activation of IL-1β. ASC expression is controlled through epigenetic modification, and lower ASC methylation is associated with worse outcomes in HF.
Hypothesis: Peak V̇O2 will be positively related to ASC methylation and negatively related to IL-1β in persons with HF.
Methods: This cross-sectional study examined the relationship between ASC methylation and the inflammatory cytokine IL-1β with peak V̇O2 in 54 stable outpatients with HF. All participants were NYHA class II or III, not currently engaged in an exercise program, and physically able to complete a symptom limited modified Balke exercise treadmill test.
Results: Participants were 59 ± 10 years of age, 52% female, and 59% African American. Mean peak V̇O2 was 16.68 ± 4.7 ml/kg/min. Peak V̇O2 was positively associated with mean percent ASC methylation (r=.47, p=.001) and negatively associated with IL-1β (r=-.38, p=.007). Multiple linear regression models controlling for left ventricular ejection fraction and gender demonstrated that peak V̇O2 increased by 2.30 ml/kg/min for every 1% increase in mean ASC methylation and decreased by 1.91 ml/kg/min for every 1 pg/mL increase in plasma IL-1β.
Conclusions: Mean percent ASC methylation and plasma IL-1β levels are associated with clinically meaningful changes in peak V̇O2 in persons with HF. Inflammasome activation may play a mechanistic role in determining aerobic capacity. ASC methylation is a potentially modifiable mechanism for reducing the inflammatory response, thereby improving aerobic capacity in HF. Modification of ASC expression via behavioral interventions that increase ASC methylation, may improve aerobic capacity in persons with HF.
Invited Talk in the Cardiovascular Seminar session: Cytokine-Targeted Therapies in Heart Failure: Where are We in 2016?
American Heart Association Scientific Sessions, November 2016, New Orleans, LA
American Heart Association Scientific Sessions, November 2016, New Orleans, LA
Heart Failure Society of America, September 2016, Orlando, FL
Effects of an Exercise Intervention on ASC Methylation and IL-1 Cytokines in Persons with Heart Failure
Introduction: Inflammation is a key factor contributing to disease progression in heart failure (HF), and the interleukin (IL)-1 cytokines IL-1β and IL-18 are implicated in this process. The adaptor protein ASC (apoptosis associated speck-like protein containing a caspase recruitment domain) is necessary for inflammasome activation of IL-1β and IL-18. ASC expression is controlled through epigenetic modification, and lower ASC methylation is associated with worse outcomes in HF. Higher ASC methylation is associated with exercise, but no studies have examined the effects of exercise on ASC methylation in persons with HF. The purpose of this study was to examine the effects of exercise on changes in ASC methylation and activation of IL-1β and IL-18 in persons with HF.
Hypothesis: We hypothesized that: 1) persons with HF who participate in a 3-month exercise intervention will have increased ASC methylation and decreased plasma IL-1β and IL-18 at completion of the intervention as compared to the control group. Further, we investigated if changes in ASC methylation, IL-1β and IL-18 were sustained 3 months after completing the exercise intervention.
Methods: Participants (N=54) were enrolled in a randomized controlled 3-month exercise intervention study and randomized to receive exercise intervention (n=38) or attention control (n=16) for 3 months. Participants were followed for an additional 3-month maintenance phase after the intervention. Measures included percent methylation of the ASC gene, plasma IL-1β and IL-18 and were obtained at baseline (BL), 3 months (3M), and 6 months (6M). Analysis included multilevel modeling to analyze inter- and intra-individual differences in measures over time and to analyze group by time effects, adjusting for covariates.
Results: ASC methylation was higher in the exercise group as compared to control at 3M (6.10 ± 0.5% vs. 5.80 ± 0.4%; p=.04) and 6M (6.07 ± 0.4 vs. 5.82 ± 0.4; p=.04), with medium to large effects sizes of .72 and .81. Plasma IL-1β was lower among the exercise group as compared to control at 3M (1.43 ± 0.5 p/mL vs. 2.09 ± 1.3 pg/mL; p=.02) and 6M (1.49 ± 0.5 pg/mL vs. 2.13 ± 1.4 pg/mL; p=.004), with medium to large effect sizes of .83 and .79. Among those in the exercise group ASC methylation was higher at 3M as compared to BL (p=.009), and IL-1β was lower than BL at both 3M (p<.001) and 6M (p=.04). Although no group differences in IL-18 were found over time, IL-1β change scores were positively associated with changes in IL-18 from BL to 3M (r=.422, p=.020) and from 3M to 6M (r=.411, p=.037).
Conclusions: A 3-month exercise intervention was related to increased mean percent ASC methylation and decreased IL-1β and ASC mRNA gene expression in persons with HF. Epigenetic regulation of ASC can be further explored as a biological mechanism by which exercise can promote better outcomes in HF. Further research examining mechanisms of change are warranted to improve understanding of physiological adaptations and more precise prediction of adverse outcomes in persons with HF.
Effects of an Exercise Intervention on ASC Methylation and IL-1 Cytokines in Persons with Heart Failure
Introduction: Inflammation is a key factor contributing to disease progression in heart failure (HF), and the interleukin (IL)-1 cytokines IL-1β and IL-18 are implicated in this process. The adaptor protein ASC (apoptosis associated speck-like protein containing a caspase recruitment domain) is necessary for inflammasome activation of IL-1β and IL-18. ASC expression is controlled through epigenetic modification, and lower ASC methylation is associated with worse outcomes in HF. Higher ASC methylation is associated with exercise, but no studies have examined the effects of exercise on ASC methylation in persons with HF. The purpose of this study was to examine the effects of exercise on changes in ASC methylation and activation of IL-1β and IL-18 in persons with HF.
Hypothesis: We hypothesized that: 1) persons with HF who participate in a 3-month exercise intervention will have increased ASC methylation and decreased plasma IL-1β and IL-18 at completion of the intervention as compared to the control group. Further, we investigated if changes in ASC methylation, IL-1β and IL-18 were sustained 3 months after completing the exercise intervention.
Methods: Participants (N=54) were enrolled in a randomized controlled 3-month exercise intervention study and randomized to receive exercise intervention (n=38) or attention control (n=16) for 3 months. Participants were followed for an additional 3-month maintenance phase after the intervention. Measures included percent methylation of the ASC gene, plasma IL-1β and IL-18 and were obtained at baseline (BL), 3 months (3M), and 6 months (6M). Analysis included multilevel modeling to analyze inter- and intra-individual differences in measures over time and to analyze group by time effects, adjusting for covariates.
Results: ASC methylation was higher in the exercise group as compared to control at 3M (6.10 ± 0.5% vs. 5.80 ± 0.4%; p=.04) and 6M (6.07 ± 0.4 vs. 5.82 ± 0.4; p=.04), with medium to large effects sizes of .72 and .81. Plasma IL-1β was lower among the exercise group as compared to control at 3M (1.43 ± 0.5 p/mL vs. 2.09 ± 1.3 pg/mL; p=.02) and 6M (1.49 ± 0.5 pg/mL vs. 2.13 ± 1.4 pg/mL; p=.004), with medium to large effect sizes of .83 and .79. Among those in the exercise group ASC methylation was higher at 3M as compared to BL (p=.009), and IL-1β was lower than BL at both 3M (p<.001) and 6M (p=.04). Although no group differences in IL-18 were found over time, IL-1β change scores were positively associated with changes in IL-18 from BL to 3M (r=.422, p=.020) and from 3M to 6M (r=.411, p=.037).
Conclusions: A 3-month exercise intervention was related to increased mean percent ASC methylation and decreased IL-1β and ASC mRNA gene expression in persons with HF. Epigenetic regulation of ASC can be further explored as a biological mechanism by which exercise can promote better outcomes in HF. Further research examining mechanisms of change are warranted to improve understanding of physiological adaptations and more precise prediction of adverse outcomes in persons with HF.
Southern Nursing Research Society, February 2016, Williamsburg, VA
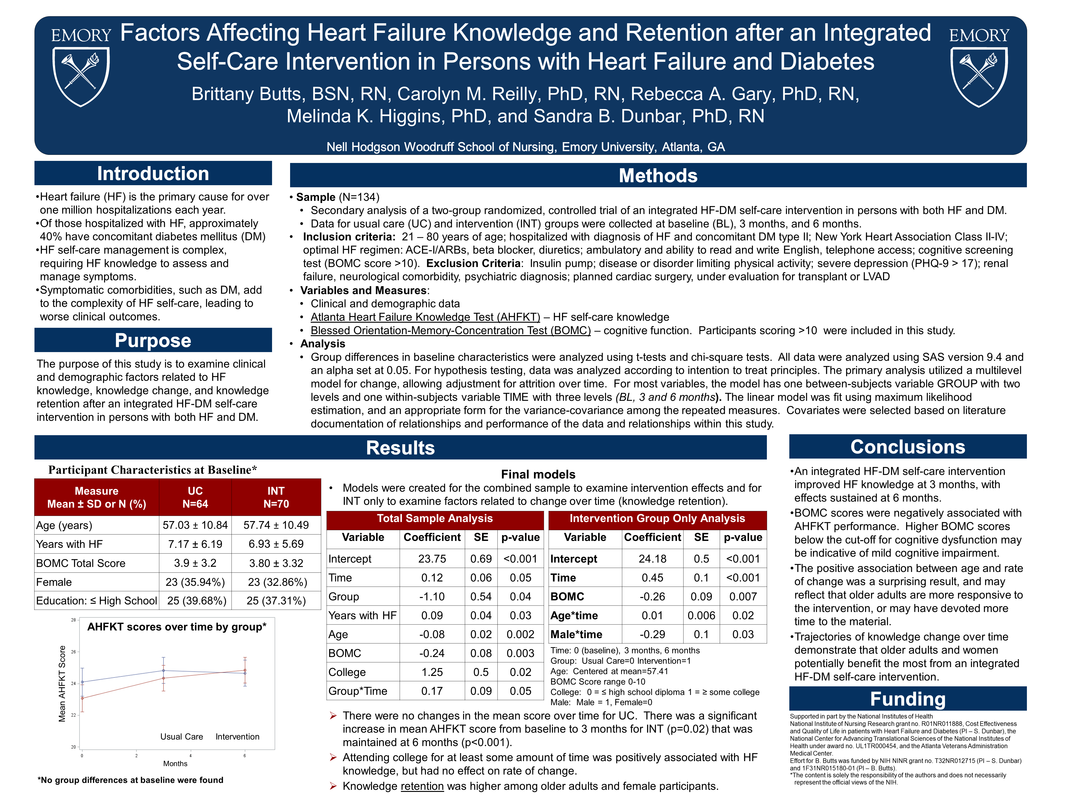
Factors Affecting Heart failure Knowledge and Retention after an Integrated Self-Care Intervention in Persons with Heart Failure and Diabetes
Brittany Butts, Carolyn Reilly, Rebecca Gary, Melinda Higgins, and Sandra Dunbar
Introduction
Heart failure (HF) is the primary cause for over one million hospitalizations each year. Of those hospitalized with HF, approximately 40% have concomitant diabetes mellitus (DM). HF self-care management is complex, requiring HF knowledge to assess and manage symptoms. Symptomatic comorbidities, such as DM, add to the complexity of HF self-care, leading to worse clinical outcomes. The purpose of this study is to examine clinical and demographic factors related to HF knowledge, knowledge change, and knowledge retention after an integrated HF-DM self-care intervention in persons with both HF and DM.
Methods
This study is a secondary analysis of a two-group randomized, controlled trial of an integrated HF-DM self-care intervention in persons with both HF and DM. The Atlanta Heart Failure Knowledge Test (AHFKT) was used to measure HF self-care knowledge. The Blessed Orientation-Memory Concentration (BOMC) test was used to screen for cognitive function; participants scoring >10 were included in this study. Data for usual care (UC) and intervention (INT) groups were collected at baseline (BL), 3 months and 6 months. Analyses included descriptive, t-test, and multilevel modeling to predict knowledge change.
Results
Participants (n=134) were mean age 57.41 ± 10.6, 34% women, 69% African American. There were no changes in mean AHFKT score over time for UC. There was a significant increase in mean AHFKT from BL to 3 months for INT (p=.02) that was maintained at 6 months (p<.001). HF knowledge scores were positively associated with time (β=0.045, p<.001) and negatively associated with BL BOMC score (β=-0.29, p=.007). Greater Knowledge retention over time was associated with older age (p=.02), and female gender (p=.02). No relationships between knowledge change and education, HF severity or number of comorbidities were found.
Discussion and Conclusions
This study demonstrated that an integrated HF-DM self-care intervention improved HF knowledge at 3 months, with effects sustained at 6 months. Trajectories of knowledge change over time demonstrate that older adults and women potentially benefit the most from an integrated HF-DM self-care intervention. Further studies to examine factors and approaches to improve HF knowledge and retention are warranted.
Factors Affecting Heart failure Knowledge and Retention after an Integrated Self-Care Intervention in Persons with Heart Failure and Diabetes
Brittany Butts, Carolyn Reilly, Rebecca Gary, Melinda Higgins, and Sandra Dunbar
Introduction
Heart failure (HF) is the primary cause for over one million hospitalizations each year. Of those hospitalized with HF, approximately 40% have concomitant diabetes mellitus (DM). HF self-care management is complex, requiring HF knowledge to assess and manage symptoms. Symptomatic comorbidities, such as DM, add to the complexity of HF self-care, leading to worse clinical outcomes. The purpose of this study is to examine clinical and demographic factors related to HF knowledge, knowledge change, and knowledge retention after an integrated HF-DM self-care intervention in persons with both HF and DM.
Methods
This study is a secondary analysis of a two-group randomized, controlled trial of an integrated HF-DM self-care intervention in persons with both HF and DM. The Atlanta Heart Failure Knowledge Test (AHFKT) was used to measure HF self-care knowledge. The Blessed Orientation-Memory Concentration (BOMC) test was used to screen for cognitive function; participants scoring >10 were included in this study. Data for usual care (UC) and intervention (INT) groups were collected at baseline (BL), 3 months and 6 months. Analyses included descriptive, t-test, and multilevel modeling to predict knowledge change.
Results
Participants (n=134) were mean age 57.41 ± 10.6, 34% women, 69% African American. There were no changes in mean AHFKT score over time for UC. There was a significant increase in mean AHFKT from BL to 3 months for INT (p=.02) that was maintained at 6 months (p<.001). HF knowledge scores were positively associated with time (β=0.045, p<.001) and negatively associated with BL BOMC score (β=-0.29, p=.007). Greater Knowledge retention over time was associated with older age (p=.02), and female gender (p=.02). No relationships between knowledge change and education, HF severity or number of comorbidities were found.
Discussion and Conclusions
This study demonstrated that an integrated HF-DM self-care intervention improved HF knowledge at 3 months, with effects sustained at 6 months. Trajectories of knowledge change over time demonstrate that older adults and women potentially benefit the most from an integrated HF-DM self-care intervention. Further studies to examine factors and approaches to improve HF knowledge and retention are warranted.
2015 Conference Presentations
American Heart Association Scientific Sessions, November 2015, Orlando, FL
ASC methylation and outcomes in heart failure
Brittany Butts, , Rebecca A. Gary, Sandra B. Dunbar, and Javed Butler
Background: Heart failure (HF) is associated with inflammation characterized by the formation of a protein complex, the inflammasome that triggers maturation of inflammatory cytokines. Inflammation in HF is associated with lower quality of life (QOL), depression, and poor outcomes. ASC, a vital component of the inflammasome, is controlled through epigenetic modification via methylation of CpG islands surrounding exon 1, and this methylation is a candidate pathway of worsening HF. The purpose of this study is to examine the relationships between ASC methylation and clinical, psychological, and QOL outcomes in HF.
Methods: Stored samples from 155 HF outpatients (age 56.9±12.0 years, 64% male, 47% black, and mean LVEF 29.9±14.9) were analyzed for % methylation of seven CpG sites in the intron region preceding exon 1 of the ASC gene using pyrosequencing of bisulfite treated genomic DNA. Clinical, QOL, and psychological outcomes were assessed. Two-year combined clinical endpoint (death, heart transplantation, ventricular assist device implantation, or all-cause hospitalization) was analyzed. Bivariate correlational and linear and logistic regression analyses were performed
Results: Mean total ASC methylation was 5.96±0.55%. ASC methylation was inversely related to ASC mRNA (r=-.33, p<0.001) and protein (r=-.464, p<.001). ASC methylation had a positive linear relationship with ejection fraction (r=.81, p<.001) and six-minute walk distance (r=.63, p=.005). ASC methylation had a negative linear relationship with depression (r=-.65, p<.001) and anxiety (r=-.53, p<.001) scores and a positive linear relationship with QOL (r=.83, p<.001). Combined clinical endpoint occurred in 71% (N=110) of participants. Higher levels of ASC methylation were associated with lower odds of clinical endpoint (odd ratio=0.43, 95% CI .187, .997, p=.049), while higher levels of ASC protein expression were associated with higher odds (OR=1.27, 95% CI 1.04,1.54, p=.016).
Conclusion: Increased methylation of CpG sites in the intron region of ASC is associated with improved clinical, psychological and QOL outcomes in HF. The associated decrease in ASC expression implicates this inflammatory mediator as a possible driver of HF outcomes, and may represent a therapeutic target.
ASC methylation and outcomes in heart failure
Brittany Butts, , Rebecca A. Gary, Sandra B. Dunbar, and Javed Butler
Background: Heart failure (HF) is associated with inflammation characterized by the formation of a protein complex, the inflammasome that triggers maturation of inflammatory cytokines. Inflammation in HF is associated with lower quality of life (QOL), depression, and poor outcomes. ASC, a vital component of the inflammasome, is controlled through epigenetic modification via methylation of CpG islands surrounding exon 1, and this methylation is a candidate pathway of worsening HF. The purpose of this study is to examine the relationships between ASC methylation and clinical, psychological, and QOL outcomes in HF.
Methods: Stored samples from 155 HF outpatients (age 56.9±12.0 years, 64% male, 47% black, and mean LVEF 29.9±14.9) were analyzed for % methylation of seven CpG sites in the intron region preceding exon 1 of the ASC gene using pyrosequencing of bisulfite treated genomic DNA. Clinical, QOL, and psychological outcomes were assessed. Two-year combined clinical endpoint (death, heart transplantation, ventricular assist device implantation, or all-cause hospitalization) was analyzed. Bivariate correlational and linear and logistic regression analyses were performed
Results: Mean total ASC methylation was 5.96±0.55%. ASC methylation was inversely related to ASC mRNA (r=-.33, p<0.001) and protein (r=-.464, p<.001). ASC methylation had a positive linear relationship with ejection fraction (r=.81, p<.001) and six-minute walk distance (r=.63, p=.005). ASC methylation had a negative linear relationship with depression (r=-.65, p<.001) and anxiety (r=-.53, p<.001) scores and a positive linear relationship with QOL (r=.83, p<.001). Combined clinical endpoint occurred in 71% (N=110) of participants. Higher levels of ASC methylation were associated with lower odds of clinical endpoint (odd ratio=0.43, 95% CI .187, .997, p=.049), while higher levels of ASC protein expression were associated with higher odds (OR=1.27, 95% CI 1.04,1.54, p=.016).
Conclusion: Increased methylation of CpG sites in the intron region of ASC is associated with improved clinical, psychological and QOL outcomes in HF. The associated decrease in ASC expression implicates this inflammatory mediator as a possible driver of HF outcomes, and may represent a therapeutic target.
American Heart Association Scientific Sessions, November 2015, Orlando, FL
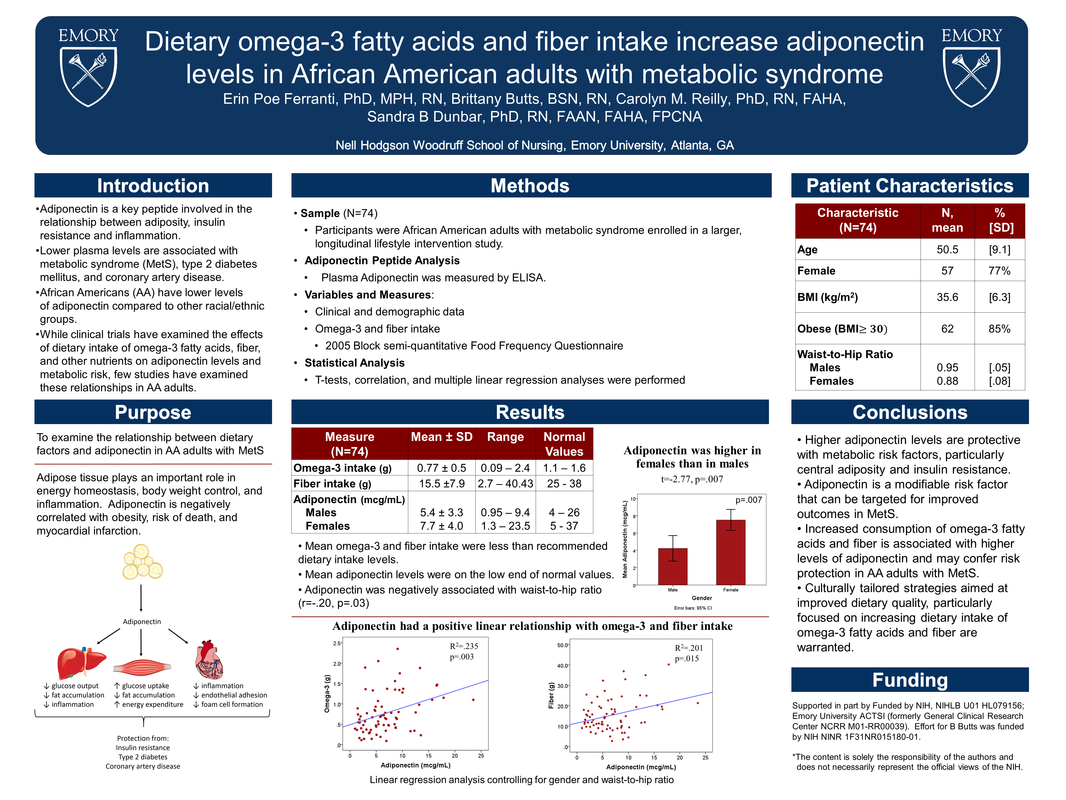
Dietary Omega-3 Fatty Acids and Fiber Intake Increase Adiponectin Levels in African American Adults with Metabolic Syndrome
Erin Ferranti, Brittany Butts, Carolyn Reilly, and Sandra Dunbar
Introduction and Purpose: Adiponectin is a key peptide involved in the relationship between adiposity, insulin resistance and inflammation. Lower plasma levels are associated with metabolic syndrome (MetS), type 2 diabetes mellitus, and coronary artery disease. African Americans (AA) have lower levels of adiponectin compared to other racial/ethnic groups. While clinical trials have examined the effects of dietary intake of omega-3 fatty acids, fiber, and other nutrients on adiponectin levels and metabolic risk, few studies have examined these relationships in AA adults. The purpose of this study is to examine the relationship between dietary factors and adiponectin in AA adults with MetS.
Methods: This analysis is of baseline data from a larger, longitudinal lifestyle intervention study in AA adults with metabolic syndrome. Dietary intake was assessed with the 2005 Block Food Frequency Questionnaire. Plasma adiponectin was measured by ELISA. Analysis included descriptive statistics, correlations and multiple regression.
Results: Seventy-four participants, 50.5±9.1 years of age, 77% female, were included in this analysis. Most participants (N=62, 85%) were obese, with mean BMI 35.6±6.3 and mean waist-hip ratio (W:H) 0.95±.05 for males and 0.88±.08 for females. Mean omega-3 intake was .77±0.5g and fiber intake was 15.47±7.9g. Adiponectin was higher in females than males (7.7±4.0 vs 5.4±3.3, t=-2.8, p=.007) and negatively associated with W:H (r=-.20, p=.03). Adiponectin had a positive linear relationship with omega-3 (R2=.235, p=.003) and fiber (R2=.201, p=.015) intake, controlling for gender and W:H. These relationships are consistent with studies in other ethnic groups.
Conclusion: Higher adiponectin levels are protective with metabolic risk factors, particularly central adiposity. Increased consumption of omega-3 fatty acids and fiber is associated with higher levels of adiponectin and may confer risk protection in AA adults with MetS. Culturally tailored strategies aimed at improved dietary quality, particularly focused on increasing dietary intake of omega-3 fatty acids and fiber are warranted.
Dietary Omega-3 Fatty Acids and Fiber Intake Increase Adiponectin Levels in African American Adults with Metabolic Syndrome
Erin Ferranti, Brittany Butts, Carolyn Reilly, and Sandra Dunbar
Introduction and Purpose: Adiponectin is a key peptide involved in the relationship between adiposity, insulin resistance and inflammation. Lower plasma levels are associated with metabolic syndrome (MetS), type 2 diabetes mellitus, and coronary artery disease. African Americans (AA) have lower levels of adiponectin compared to other racial/ethnic groups. While clinical trials have examined the effects of dietary intake of omega-3 fatty acids, fiber, and other nutrients on adiponectin levels and metabolic risk, few studies have examined these relationships in AA adults. The purpose of this study is to examine the relationship between dietary factors and adiponectin in AA adults with MetS.
Methods: This analysis is of baseline data from a larger, longitudinal lifestyle intervention study in AA adults with metabolic syndrome. Dietary intake was assessed with the 2005 Block Food Frequency Questionnaire. Plasma adiponectin was measured by ELISA. Analysis included descriptive statistics, correlations and multiple regression.
Results: Seventy-four participants, 50.5±9.1 years of age, 77% female, were included in this analysis. Most participants (N=62, 85%) were obese, with mean BMI 35.6±6.3 and mean waist-hip ratio (W:H) 0.95±.05 for males and 0.88±.08 for females. Mean omega-3 intake was .77±0.5g and fiber intake was 15.47±7.9g. Adiponectin was higher in females than males (7.7±4.0 vs 5.4±3.3, t=-2.8, p=.007) and negatively associated with W:H (r=-.20, p=.03). Adiponectin had a positive linear relationship with omega-3 (R2=.235, p=.003) and fiber (R2=.201, p=.015) intake, controlling for gender and W:H. These relationships are consistent with studies in other ethnic groups.
Conclusion: Higher adiponectin levels are protective with metabolic risk factors, particularly central adiposity. Increased consumption of omega-3 fatty acids and fiber is associated with higher levels of adiponectin and may confer risk protection in AA adults with MetS. Culturally tailored strategies aimed at improved dietary quality, particularly focused on increasing dietary intake of omega-3 fatty acids and fiber are warranted.
Heart Failure Society of America, September 2015, National Harbor Maryland
ASC Methylation and Expression are Associated with Depressive Symptoms, Anxiety, and Quality of Life in Heart Failure
Brittany Butts, Rebecca Gary, Sandra Dunbar, and Javed Butler
Introduction: Heart failure (HF) is associated with a chronic, low-grade inflammation characterized by the formation and activation of the inflammasome, a complex of intracellular interaction proteins that trigger maturation of inflammatory cytokines to initiate the inflammatory response. Increased inflammation in HF is associated with lower quality of life (QOL) and higher rates of depressive symptoms, leading to poor clinical outcomes. ASC, a vital component of the inflammasome, is controlled through epigenetic modification via methylation of CpG islands surrounding exon 1, and this methylation is a likely candidate pathway in the pathophysiology of HF. The specific mechanisms of these relationships are not known. This study examined relationships between ASC methylation and psychological and QOL outcomes.
Hypothesis: Levels of ASC methylation will be inversely correlated with depressive symptoms and anxiety and positively correlated with QOL.
Methods: Stored samples (n=155) from a cohort of outpatients with HF, mean age 56.89 ± 12.0 years, 64% male, 47% African American, and mean LVEF 29.94 ± 14.9 were analyzed for percent methylation of seven CpG sites in the intron region preceding exon 1 of the ASC gene using pyrosequencing of bisulfite treated genomic DNA. Variables and measures include demographics, clinical data, QOL (Kansas City Cardiomyopathy Questionnaire [KCCQ]), anxiety (Generalized Anxiety Disorder Scale [GAD-7]), and depressive symptoms (Patient Health Questionnaire [PHQ-9]). Descriptive, correlational and linear regression analyses were performed, controlling for age, gender, race, BMI, and LVEF.
Results: Mean total ASC methylation was 5.96 ± 0.55%. Total ASC methylation was inversely related to ASC mRNA (r=-.33, p<0.001) and protein (r=-.464, p<.001). Total ASC methylation had a negative linear relationship with PHQ-9 scores (r=-.65, p<.001) and GAD-7 (r=-.53, p<.001) scores and a positive linear relationship with KCCQ scores (r=.83, p<.001). Higher ASC gene expression had small to moderate associations with higher PHQ-9 scores (r=.20, p=.02) and lower QOL (r=-.32, p<.001).
Discussion & Conclusion: Increased methylation of CpG sites in the intron region of ASC is associated with improved psychological and quality of life outcomes in persons with HF. The associated decrease in ASC expression implicates this inflammatory mediator as a possible driver of HF outcomes. Modification of ASC expression, such as behavioral interventions that increase ASC methylation, may improve outcomes in persons with HF.
ASC Methylation and Expression are Associated with Depressive Symptoms, Anxiety, and Quality of Life in Heart Failure
Brittany Butts, Rebecca Gary, Sandra Dunbar, and Javed Butler
Introduction: Heart failure (HF) is associated with a chronic, low-grade inflammation characterized by the formation and activation of the inflammasome, a complex of intracellular interaction proteins that trigger maturation of inflammatory cytokines to initiate the inflammatory response. Increased inflammation in HF is associated with lower quality of life (QOL) and higher rates of depressive symptoms, leading to poor clinical outcomes. ASC, a vital component of the inflammasome, is controlled through epigenetic modification via methylation of CpG islands surrounding exon 1, and this methylation is a likely candidate pathway in the pathophysiology of HF. The specific mechanisms of these relationships are not known. This study examined relationships between ASC methylation and psychological and QOL outcomes.
Hypothesis: Levels of ASC methylation will be inversely correlated with depressive symptoms and anxiety and positively correlated with QOL.
Methods: Stored samples (n=155) from a cohort of outpatients with HF, mean age 56.89 ± 12.0 years, 64% male, 47% African American, and mean LVEF 29.94 ± 14.9 were analyzed for percent methylation of seven CpG sites in the intron region preceding exon 1 of the ASC gene using pyrosequencing of bisulfite treated genomic DNA. Variables and measures include demographics, clinical data, QOL (Kansas City Cardiomyopathy Questionnaire [KCCQ]), anxiety (Generalized Anxiety Disorder Scale [GAD-7]), and depressive symptoms (Patient Health Questionnaire [PHQ-9]). Descriptive, correlational and linear regression analyses were performed, controlling for age, gender, race, BMI, and LVEF.
Results: Mean total ASC methylation was 5.96 ± 0.55%. Total ASC methylation was inversely related to ASC mRNA (r=-.33, p<0.001) and protein (r=-.464, p<.001). Total ASC methylation had a negative linear relationship with PHQ-9 scores (r=-.65, p<.001) and GAD-7 (r=-.53, p<.001) scores and a positive linear relationship with KCCQ scores (r=.83, p<.001). Higher ASC gene expression had small to moderate associations with higher PHQ-9 scores (r=.20, p=.02) and lower QOL (r=-.32, p<.001).
Discussion & Conclusion: Increased methylation of CpG sites in the intron region of ASC is associated with improved psychological and quality of life outcomes in persons with HF. The associated decrease in ASC expression implicates this inflammatory mediator as a possible driver of HF outcomes. Modification of ASC expression, such as behavioral interventions that increase ASC methylation, may improve outcomes in persons with HF.
Basic Cardiovascular Sciences Scientific Sessions, July 2015, New Orleans, LA
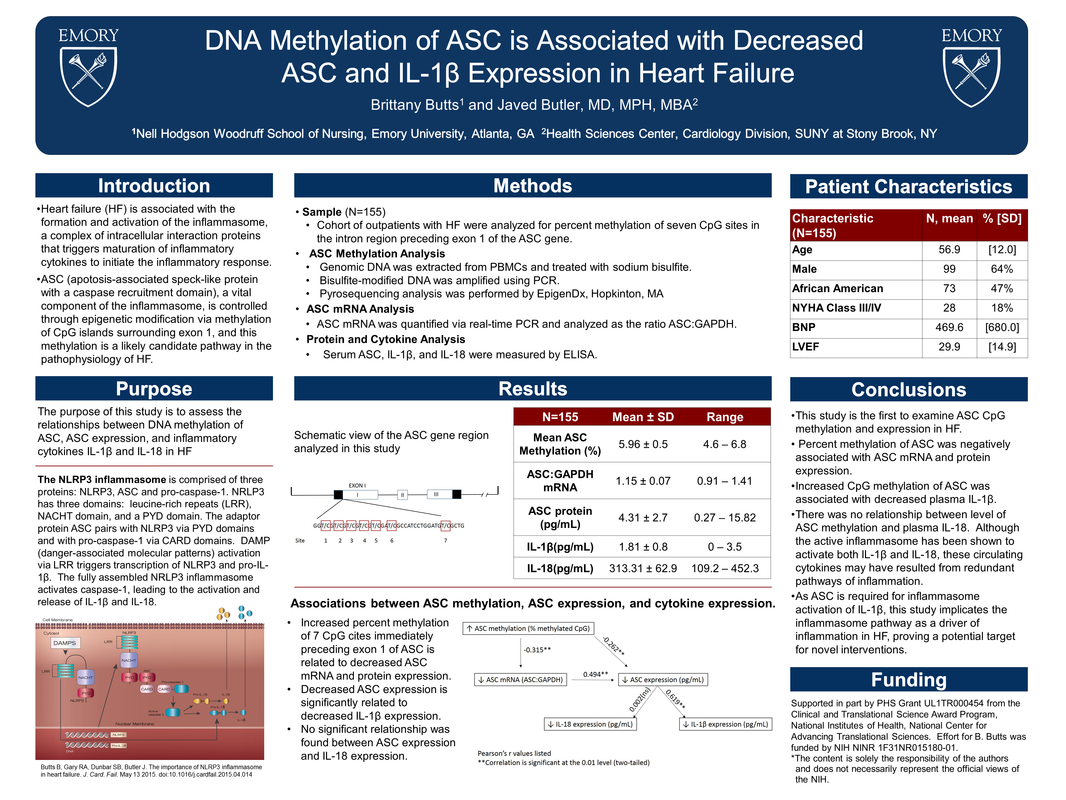
DNA Methylation of ASC is Associated with Decreased ASC and IL-1β Expression in Heart Failure
Brittany Butts and Javed Butler
Introduction: Heart failure (HF) is associated with formation and activation of inflammasome, a complex of intracellular interaction proteins that trigger maturation of inflammatory cytokines to initiate inflammatory response. ASC, a vital component of the inflammasome, is controlled through epigenetic modification via methylation of CpG islands surrounding exon 1.
Methods: To assess the relationships between DNA methylation of ASC, ASC expression, and inflammatory cytokines IL-1β and IL-18 in HF, stored samples from 155 chronic HF patients (age 56.9±12.0 yr, 64% male, 47% black, and ejection fraction 29.9±14.9) were analyzed. DNA extracted from PMBCs were analyzed by pyrosequencing for percent methylation of seven CpG sites in the intron region preceding exon 1 of the ASC gene. ASC mRNA was quantified via real-time PCR and analyzed as the ratio ASC:GAPDH. Serum ASC, IL-1β, and IL-18 were measured by ELISA.
Results: Higher ASC methylation was associated with lower ASC mRNA (r=0-.328, p<0.001) and protein (r=-.464, p<0.001) expression. Lower ASC mRNA expression was associated with lower ASC protein expression (r=0.494, p<0.001). Decreased IL-1β expression was associated with higher ASC methylation (r=-.424, p=0.005) and lower ASC mRNA (r=.619, p<0.001) and ASC protein (r=.433, p<0.001). IL-18 expression was not significantly associated with ASC methylation or expression.
Conclusions: Increased ASC methylation was associated with lower IL-1β, likely via decreased ASC gene expression. As ASC is required for inflammasome activation of IL-1β, this study implicates the inflammasome pathway as a driver of inflammation in HF, proving a potential target for novel interventions.
DNA Methylation of ASC is Associated with Decreased ASC and IL-1β Expression in Heart Failure
Brittany Butts and Javed Butler
Introduction: Heart failure (HF) is associated with formation and activation of inflammasome, a complex of intracellular interaction proteins that trigger maturation of inflammatory cytokines to initiate inflammatory response. ASC, a vital component of the inflammasome, is controlled through epigenetic modification via methylation of CpG islands surrounding exon 1.
Methods: To assess the relationships between DNA methylation of ASC, ASC expression, and inflammatory cytokines IL-1β and IL-18 in HF, stored samples from 155 chronic HF patients (age 56.9±12.0 yr, 64% male, 47% black, and ejection fraction 29.9±14.9) were analyzed. DNA extracted from PMBCs were analyzed by pyrosequencing for percent methylation of seven CpG sites in the intron region preceding exon 1 of the ASC gene. ASC mRNA was quantified via real-time PCR and analyzed as the ratio ASC:GAPDH. Serum ASC, IL-1β, and IL-18 were measured by ELISA.
Results: Higher ASC methylation was associated with lower ASC mRNA (r=0-.328, p<0.001) and protein (r=-.464, p<0.001) expression. Lower ASC mRNA expression was associated with lower ASC protein expression (r=0.494, p<0.001). Decreased IL-1β expression was associated with higher ASC methylation (r=-.424, p=0.005) and lower ASC mRNA (r=.619, p<0.001) and ASC protein (r=.433, p<0.001). IL-18 expression was not significantly associated with ASC methylation or expression.
Conclusions: Increased ASC methylation was associated with lower IL-1β, likely via decreased ASC gene expression. As ASC is required for inflammasome activation of IL-1β, this study implicates the inflammasome pathway as a driver of inflammation in HF, proving a potential target for novel interventions.
Southern Nursing Research Society, February 2015, Tampa, FL
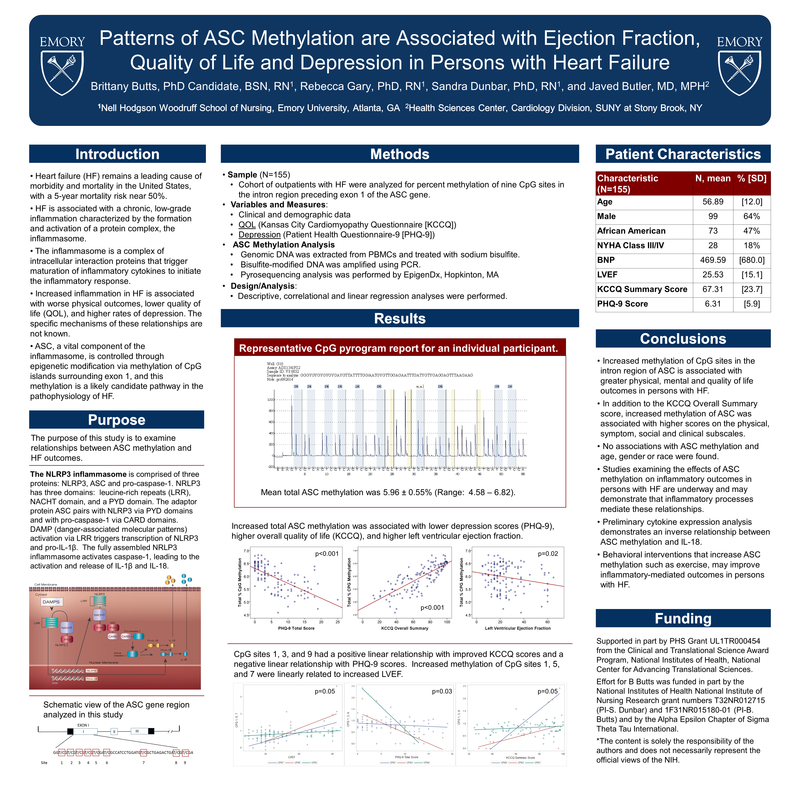
Patterns of ASC Methylation are Associated with Ejection Fraction, Quality of Life and Depression in Persons with Heart Failure
Brittany Butts, Rebecca Gary, Sandra Dunbar, and Javed Butler
Introduction: Heart failure (HF) remains a leading cause of morbidity and mortality in the United States, with a 5-year mortality risk near 50%. HF is associated with a chronic, low-grade inflammation characterized by the formation and activation of a protein complex, the inflammasome. The inflammasome is a complex of intracellular interaction proteins that trigger maturation of inflammatory cytokines to initiate the inflammatory response. Increased inflammation in HF is associated with worse physical outcomes, lower quality of life (QOL), and higher rates of depression. ASC, a vital component of the inflammasome, is controlled through epigenetic modification via methylation of CpG islands surrounding exon 1. The purpose of this study is to examine relationships between ASC methylation and HF outcomes.
Methods: Stored samples (n=90) from a cohort of outpatients with HF, mean age 56.64±12.6 years, 57% male, 48.96% African American, and mean LVEF 31.06±16.05 were analyzed for percent methylation of nine CpG sites in the intron region preceding exon 1 of the ASC gene. Variables and measures include demographics, clinical data, QOL (Kansas City Cardiomyopathy Questionnaire [KCCQ]) and depression (Patient Health Questionnaire [PHQ-9]). Descriptive, correlational and linear regression analyses were performed.
Results: Mean total ASC methylation was 5.41 ± 5.55% (median 3.45, IQR 2.5–5.9). Total ASC methylation had a positive linear relationship with BNP (p=0.05), controlling for age and LVEF. Increased methylation of CpG sites 1, 3 and 9 had a positive linear relationship with improved KCCQ scores (p=0.05) and a negative linear relationship with PHQ-9 scores (p=0.03). Increased methylation of CpG sites 1, 5 and 7 were linearly related to increased LFEV (p=0.05). No differences in age or gender were found.
Discussion & Conclusion: Increased methylation of CpG sites in the intron region of ASC is associated with improved physical, mental and quality of life outcomes in persons with HF. Studies examining the effects of ASC methylation on inflammatory outcomes in persons with HF are underway and may demonstrate that inflammatory processes mediate this relationship. Behavioral interventions that increase ASC methylation may improve outcomes in persons with HF.
Patterns of ASC Methylation are Associated with Ejection Fraction, Quality of Life and Depression in Persons with Heart Failure
Brittany Butts, Rebecca Gary, Sandra Dunbar, and Javed Butler
Introduction: Heart failure (HF) remains a leading cause of morbidity and mortality in the United States, with a 5-year mortality risk near 50%. HF is associated with a chronic, low-grade inflammation characterized by the formation and activation of a protein complex, the inflammasome. The inflammasome is a complex of intracellular interaction proteins that trigger maturation of inflammatory cytokines to initiate the inflammatory response. Increased inflammation in HF is associated with worse physical outcomes, lower quality of life (QOL), and higher rates of depression. ASC, a vital component of the inflammasome, is controlled through epigenetic modification via methylation of CpG islands surrounding exon 1. The purpose of this study is to examine relationships between ASC methylation and HF outcomes.
Methods: Stored samples (n=90) from a cohort of outpatients with HF, mean age 56.64±12.6 years, 57% male, 48.96% African American, and mean LVEF 31.06±16.05 were analyzed for percent methylation of nine CpG sites in the intron region preceding exon 1 of the ASC gene. Variables and measures include demographics, clinical data, QOL (Kansas City Cardiomyopathy Questionnaire [KCCQ]) and depression (Patient Health Questionnaire [PHQ-9]). Descriptive, correlational and linear regression analyses were performed.
Results: Mean total ASC methylation was 5.41 ± 5.55% (median 3.45, IQR 2.5–5.9). Total ASC methylation had a positive linear relationship with BNP (p=0.05), controlling for age and LVEF. Increased methylation of CpG sites 1, 3 and 9 had a positive linear relationship with improved KCCQ scores (p=0.05) and a negative linear relationship with PHQ-9 scores (p=0.03). Increased methylation of CpG sites 1, 5 and 7 were linearly related to increased LFEV (p=0.05). No differences in age or gender were found.
Discussion & Conclusion: Increased methylation of CpG sites in the intron region of ASC is associated with improved physical, mental and quality of life outcomes in persons with HF. Studies examining the effects of ASC methylation on inflammatory outcomes in persons with HF are underway and may demonstrate that inflammatory processes mediate this relationship. Behavioral interventions that increase ASC methylation may improve outcomes in persons with HF.
2014 Conference Presentations
American Heart Association Scientific Sessions, November 2017, Chicago, IL
Introduction: Frailty is a common condition in the elderly and a powerful predictor of mortality in CVD. In heart failure (HF), frailty has been shown to predict falls, disability, hospitalization and to substantially lower health related quality of life. Persons with HF are 6-7 times more likely to be frail than their age matched counterparts; the risk of frailty increases with multiple chronic conditions. Although 30-47% of persons with HF have concomitant type 2 diabetes mellitus (DM), frailty in persons with HF and DM has not been reported. The purpose of this study is to examine the effects of an integrated intervention on risk of frailty in persons with HF and DM.
Methods: A secondary analysis of a randomized, controlled, repeated measures 6-month intervention trial was performed. Persons with HF and DM (n=102), mean age 58.14 ± 10.3 years, 69% male, 66% African American, and mean LVEF 34.72 ± 17.5 were randomized into usual care (UC) or an integrated HF-DM self-care education/counseling (HF-DM-SC) group which provided HF-DM self-care education and skills, psychosocial counseling to increase HF and DM self-efficacy, enhanced physical activity through walking, and facilitated decision making. Baseline and 6-month data were examined. Frailty was defined as total distance <300 meters on the six-minute walk test (6MWT). Descriptive, t-test, and repeated-measures ANOVA statistical analyses were used.
Results: At baseline, 60% of participants were classified as frail. Mean age (59.82) was higher (t=-2.001, p=.05) in the frail group compared with those considered not frail (55.58). No group differences in frailty were found at baseline (p=.55); frailty was not associated with BMI, LVEF, NYHA class, or comorbidities. After the 6-month HF-DM-SC intervention, the percent considered frail in the intervention group decreased from 56% to 29% while frailty in the UC group increased from 63.5% to 65% (p=0.021). No differences in age between frail and non-frail remained at 6 months.
Discussion: Frailty increases the risk of adverse outcome in persons with HF and is not limited to the elderly in persons with HF and HF-DM. An integrated self-care intervention which emphasizes increased walking and physical activity can improve frailty risk and outcomes in persons with HF-DM.
Introduction: Frailty is a common condition in the elderly and a powerful predictor of mortality in CVD. In heart failure (HF), frailty has been shown to predict falls, disability, hospitalization and to substantially lower health related quality of life. Persons with HF are 6-7 times more likely to be frail than their age matched counterparts; the risk of frailty increases with multiple chronic conditions. Although 30-47% of persons with HF have concomitant type 2 diabetes mellitus (DM), frailty in persons with HF and DM has not been reported. The purpose of this study is to examine the effects of an integrated intervention on risk of frailty in persons with HF and DM.
Methods: A secondary analysis of a randomized, controlled, repeated measures 6-month intervention trial was performed. Persons with HF and DM (n=102), mean age 58.14 ± 10.3 years, 69% male, 66% African American, and mean LVEF 34.72 ± 17.5 were randomized into usual care (UC) or an integrated HF-DM self-care education/counseling (HF-DM-SC) group which provided HF-DM self-care education and skills, psychosocial counseling to increase HF and DM self-efficacy, enhanced physical activity through walking, and facilitated decision making. Baseline and 6-month data were examined. Frailty was defined as total distance <300 meters on the six-minute walk test (6MWT). Descriptive, t-test, and repeated-measures ANOVA statistical analyses were used.
Results: At baseline, 60% of participants were classified as frail. Mean age (59.82) was higher (t=-2.001, p=.05) in the frail group compared with those considered not frail (55.58). No group differences in frailty were found at baseline (p=.55); frailty was not associated with BMI, LVEF, NYHA class, or comorbidities. After the 6-month HF-DM-SC intervention, the percent considered frail in the intervention group decreased from 56% to 29% while frailty in the UC group increased from 63.5% to 65% (p=0.021). No differences in age between frail and non-frail remained at 6 months.
Discussion: Frailty increases the risk of adverse outcome in persons with HF and is not limited to the elderly in persons with HF and HF-DM. An integrated self-care intervention which emphasizes increased walking and physical activity can improve frailty risk and outcomes in persons with HF-DM.
Preventive Cardiovascular Nurses Association, April 2014, Atlanta, GA
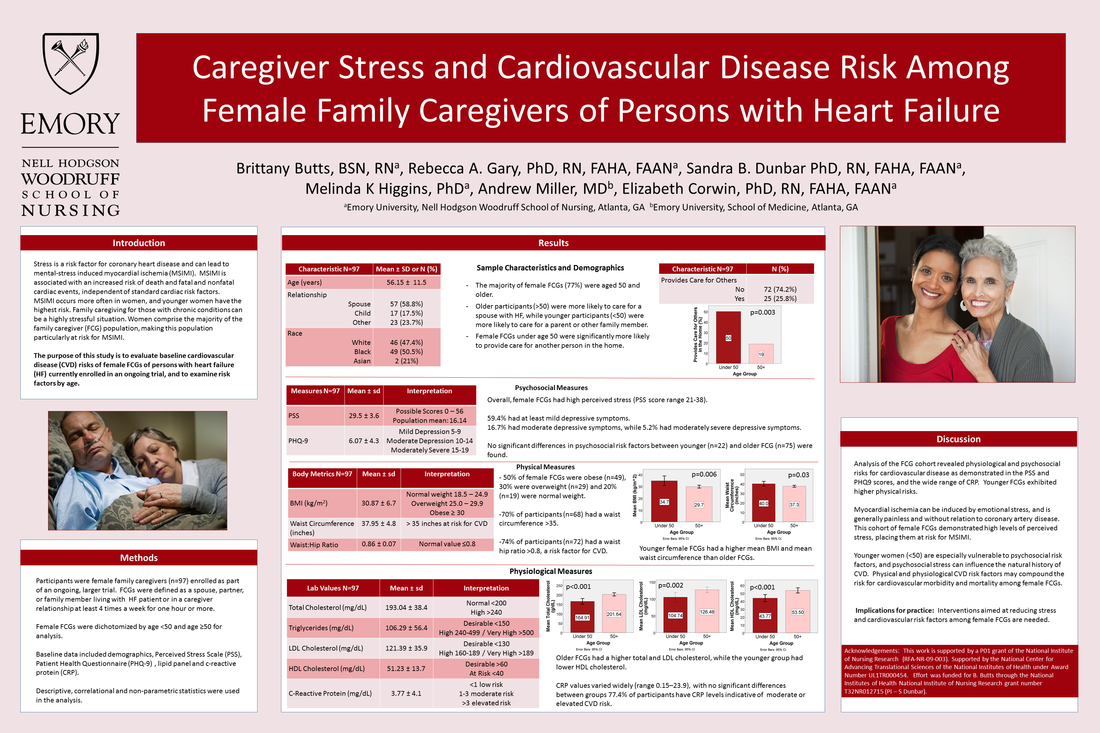
Caregiver stress and cardiovascular disease risk among female family caregivers of persons with heart failure
Brittany Butts, Rebecca Gary, Sandra B. Dunbar, Melinda K Higgins, Andrew Miller, and Elizabeth Corwin
Background: Caregiver stress is a risk factor for coronary heart disease and can lead to mental-stress induced myocardial ischemia (MSIMI). MSIMI is associated with an increased risk of death and fatal and nonfatal cardiac events, independent of standard cardiac risk factors. MSIMI occurs more often in women, and younger women have the highest risk. Women comprise the majority of the family caregiver (FCG) population, making this population particularly at risk for MSIMI.
Purpose: To evaluate baseline cardiovascular disease (CVD) risks of female FCG of persons with heart failure (HF) currently enrolled in an ongoing trial.
Methods: Female FCGs (n= 97), mean age of 56.15 ± 11.5, were dichotomized by age <50 and age ≥50. Baseline data included: Perceived Stress Scale (PSS), Patient Health Questionnaire (PHQ-9), lipid panel and c-reactive protein (CRP). Descriptive, correlational and non-parametric statistics were used in the analysis.
Results: Female FCGs had high perceived stress (PSS=29.5±3.6) and mild depressive symptoms (PHQ9=6.1±4.2); no significant differences between younger (n=22) and older FCG (n=75) were found. CRP (3.8±4.1) was elevated in both groups. Younger FCGs were more likely to care for additional people (p=0.003), have a higher BMI (p=0.006), and higher hip (p=0.05) and waist circumferences (p=0.03). Older FCGs had a higher total (p<0.001) and LDL cholesterol (p=0.002). The younger group had lower HDL cholesterol (43.7 vs 53.5, p<0.0001), demonstrating a higher CVD risk.
Conclusions: Analysis of the FCG cohort revealed physiological, physical and psychosocial risks for cardiovascular disease. PSS scores (range 21–38) exceeded the cut point for high stress for all FCGs, and the majority of participants (59.4%) exhibited at least mild depressive symptoms. CRP was high with a wide range (0.15–23.9), indicative of a heightened risk for CVD. Younger FCGs exhibited higher physical risks.
Implications for practice: Interventions aimed at reducing stress and cardiovascular risk factors among female FCGs are warranted.
Caregiver stress and cardiovascular disease risk among female family caregivers of persons with heart failure
Brittany Butts, Rebecca Gary, Sandra B. Dunbar, Melinda K Higgins, Andrew Miller, and Elizabeth Corwin
Background: Caregiver stress is a risk factor for coronary heart disease and can lead to mental-stress induced myocardial ischemia (MSIMI). MSIMI is associated with an increased risk of death and fatal and nonfatal cardiac events, independent of standard cardiac risk factors. MSIMI occurs more often in women, and younger women have the highest risk. Women comprise the majority of the family caregiver (FCG) population, making this population particularly at risk for MSIMI.
Purpose: To evaluate baseline cardiovascular disease (CVD) risks of female FCG of persons with heart failure (HF) currently enrolled in an ongoing trial.
Methods: Female FCGs (n= 97), mean age of 56.15 ± 11.5, were dichotomized by age <50 and age ≥50. Baseline data included: Perceived Stress Scale (PSS), Patient Health Questionnaire (PHQ-9), lipid panel and c-reactive protein (CRP). Descriptive, correlational and non-parametric statistics were used in the analysis.
Results: Female FCGs had high perceived stress (PSS=29.5±3.6) and mild depressive symptoms (PHQ9=6.1±4.2); no significant differences between younger (n=22) and older FCG (n=75) were found. CRP (3.8±4.1) was elevated in both groups. Younger FCGs were more likely to care for additional people (p=0.003), have a higher BMI (p=0.006), and higher hip (p=0.05) and waist circumferences (p=0.03). Older FCGs had a higher total (p<0.001) and LDL cholesterol (p=0.002). The younger group had lower HDL cholesterol (43.7 vs 53.5, p<0.0001), demonstrating a higher CVD risk.
Conclusions: Analysis of the FCG cohort revealed physiological, physical and psychosocial risks for cardiovascular disease. PSS scores (range 21–38) exceeded the cut point for high stress for all FCGs, and the majority of participants (59.4%) exhibited at least mild depressive symptoms. CRP was high with a wide range (0.15–23.9), indicative of a heightened risk for CVD. Younger FCGs exhibited higher physical risks.
Implications for practice: Interventions aimed at reducing stress and cardiovascular risk factors among female FCGs are warranted.
Southern Nursing Research Society, February 2014, San Antonio, TX
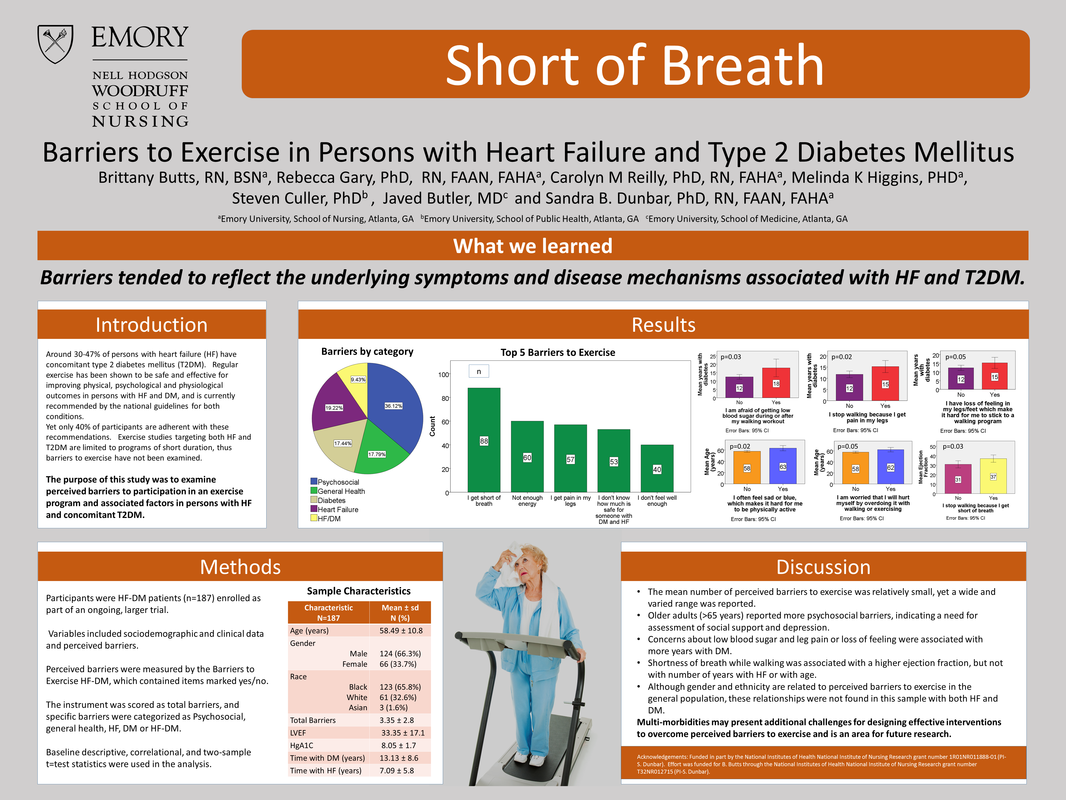
Barriers to Exercise in Persons with Heart Failure and Type 2 Diabetes Mellitus
Brittany Butts, Rebecca Gary, Carolyn Reilly, Melinda Higgins, Steven Culler, Javed Butler, and Sandra Dunbar.
Introduction: Around 30-47% of persons with heart failure (HF) have concomitant type 2 diabetes mellitus (T2DM). Regular exercise has been shown to be safe and effective for improving physical, psychological and physiological outcomes in persons with HF and DM, and is currently recommended by the national guidelines for both conditions. Yet only 40% of participants are adherent with these recommendations. Exercise studies targeting both HF and T2DM are limited to programs of short duration, thus barriers to exercise have not been examined. The purpose of this study was to examine perceived barriers to participation in an exercise program and associated factors in persons with HF and concomitant T2DM.
Methods: Participants were HF-DM patients (n=187) enrolled as part of an ongoing, larger trial. The mean age was 58.5 ± 10.8 years, 66% male, and 66% African American. Variables included sociodemographic and clinical data and perceived barriers. Perceived barriers were measured by the Barriers to Exercise HF-DM, which contained items marked yes/no. Baseline descriptive and correlational statistics were used in the analysis.
Results: The mean number of perceived exercise barriers was 3.3 ± 3 (range, 0-14). The most frequently reported barrier was shortness of breath (47%), followed by not having the energy to move around during the day (32%) and pain in legs (31%). Participants >65 years were more likely to report feeling sad and blue (p=.001), did not want to exercise alone (p=.04) and reported worries of being hurt by overdoing it (p=.04) than those <65 years. Participants stating they stopped walking due to shortness of breath had a higher LVEF (p=.05), which may reflect HF etiology. T2DM diagnosis preceded HF diagnosis in 76% of participants; this was significantly associated with reporting pain in legs (p=.04) and loss of feeling in legs/feet (p=.02).
Discussion & Conclusion: The mean number of perceived barriers to exercise was relatively small, yet a wide and varied range was reported. Barriers tended to reflect the underlying symptom and disease mechanisms associated with HF and T2DM. Thus, multi-morbidities may present additional challenges for designing effective interventions to overcome perceived barriers to exercise and is an area for future research.
Barriers to Exercise in Persons with Heart Failure and Type 2 Diabetes Mellitus
Brittany Butts, Rebecca Gary, Carolyn Reilly, Melinda Higgins, Steven Culler, Javed Butler, and Sandra Dunbar.
Introduction: Around 30-47% of persons with heart failure (HF) have concomitant type 2 diabetes mellitus (T2DM). Regular exercise has been shown to be safe and effective for improving physical, psychological and physiological outcomes in persons with HF and DM, and is currently recommended by the national guidelines for both conditions. Yet only 40% of participants are adherent with these recommendations. Exercise studies targeting both HF and T2DM are limited to programs of short duration, thus barriers to exercise have not been examined. The purpose of this study was to examine perceived barriers to participation in an exercise program and associated factors in persons with HF and concomitant T2DM.
Methods: Participants were HF-DM patients (n=187) enrolled as part of an ongoing, larger trial. The mean age was 58.5 ± 10.8 years, 66% male, and 66% African American. Variables included sociodemographic and clinical data and perceived barriers. Perceived barriers were measured by the Barriers to Exercise HF-DM, which contained items marked yes/no. Baseline descriptive and correlational statistics were used in the analysis.
Results: The mean number of perceived exercise barriers was 3.3 ± 3 (range, 0-14). The most frequently reported barrier was shortness of breath (47%), followed by not having the energy to move around during the day (32%) and pain in legs (31%). Participants >65 years were more likely to report feeling sad and blue (p=.001), did not want to exercise alone (p=.04) and reported worries of being hurt by overdoing it (p=.04) than those <65 years. Participants stating they stopped walking due to shortness of breath had a higher LVEF (p=.05), which may reflect HF etiology. T2DM diagnosis preceded HF diagnosis in 76% of participants; this was significantly associated with reporting pain in legs (p=.04) and loss of feeling in legs/feet (p=.02).
Discussion & Conclusion: The mean number of perceived barriers to exercise was relatively small, yet a wide and varied range was reported. Barriers tended to reflect the underlying symptom and disease mechanisms associated with HF and T2DM. Thus, multi-morbidities may present additional challenges for designing effective interventions to overcome perceived barriers to exercise and is an area for future research.
2013 Conference Presentations
Southern Nursing Research Society, February 2013, Little Rock, AR
Effect of an integrated heart failure and diabetes self-care intervention on quality of life and self-care behaviors
Brittany Butts, Carolyn Reilly, Melinda Higgins, Steven Cullar, Javed Butler, and Sandra Dunbar
Introduction: Studies show 30-47% of persons with heart failure (HF) have concomitant diabetes mellitus (DM). Self care for persons with these chronic conditions is conflicting, complex and often inadequate. Quality of life (QOL) may also be influenced by HF-DM and self-care. The aim of this study was to test an integrated HF and DM self-care education and counseling program intervention for its effects on HF and DM self-care behaviors and QOL and examine relationships between change in HF and DM self care and QOL.
Methods: Hospitalized HF-DM participants (n=71), mean age 60.4 years, 68.7% men, 61.2% minority, were randomized to usual care (UC) or intervention (I) using a 1:2 allocation and followed at 30 and 90 days. Intervention was an integrated education and counseling program focused on HF-DM self-care. Variables and measures were demographic and clinical data, HF and DM QOL (Minnesota Living with Heart Failure Questionnaire [MLHFQ], Audit of Diabetes-Dependent Quality of Life [ADDQOL]), HF self-care behaviors (Self-Care Heart Failure Inventory Maintenance subscale [SCHFI-m]), and DM self-care behaviors (Summary of Diabetes Self Care Assessment). Descriptive statistics and mixed models with post-hoc testing and effect size calculations were used in the analysis.
Results: At 30 days, I group exhibited improved overall HF self-care behaviors (p<.001) and improved exercise (p=.01) over baseline. At 90 days, I group had improved physical QOL as measured by the MLHFQ Physical Score (p=.02), improved foot care (p=.04) and exercise (p=.01) over baseline. Effect sizes were small to moderate. In addition, change in SCHFI-m score in the I group at 90 days was significantly associated with total HF QOL (r=.51, p=.036). No significant group or time effect was noted on the ADDQOL.
Discussion and conclusions: An integrated HF-DM self-care intervention was effective in improving essential components of self-care, including exercise and foot care behavior and perceived physical aspect of HF physical QOL. Improving overall self-care behaviors was associated with improved HF QOL. These relationships were not observed for the DM QOL and self-care variables. Future studies testing HF-DM integrated self-care interventions with longer follow up in a larger sample are warranted.
Effect of an integrated heart failure and diabetes self-care intervention on quality of life and self-care behaviors
Brittany Butts, Carolyn Reilly, Melinda Higgins, Steven Cullar, Javed Butler, and Sandra Dunbar
Introduction: Studies show 30-47% of persons with heart failure (HF) have concomitant diabetes mellitus (DM). Self care for persons with these chronic conditions is conflicting, complex and often inadequate. Quality of life (QOL) may also be influenced by HF-DM and self-care. The aim of this study was to test an integrated HF and DM self-care education and counseling program intervention for its effects on HF and DM self-care behaviors and QOL and examine relationships between change in HF and DM self care and QOL.
Methods: Hospitalized HF-DM participants (n=71), mean age 60.4 years, 68.7% men, 61.2% minority, were randomized to usual care (UC) or intervention (I) using a 1:2 allocation and followed at 30 and 90 days. Intervention was an integrated education and counseling program focused on HF-DM self-care. Variables and measures were demographic and clinical data, HF and DM QOL (Minnesota Living with Heart Failure Questionnaire [MLHFQ], Audit of Diabetes-Dependent Quality of Life [ADDQOL]), HF self-care behaviors (Self-Care Heart Failure Inventory Maintenance subscale [SCHFI-m]), and DM self-care behaviors (Summary of Diabetes Self Care Assessment). Descriptive statistics and mixed models with post-hoc testing and effect size calculations were used in the analysis.
Results: At 30 days, I group exhibited improved overall HF self-care behaviors (p<.001) and improved exercise (p=.01) over baseline. At 90 days, I group had improved physical QOL as measured by the MLHFQ Physical Score (p=.02), improved foot care (p=.04) and exercise (p=.01) over baseline. Effect sizes were small to moderate. In addition, change in SCHFI-m score in the I group at 90 days was significantly associated with total HF QOL (r=.51, p=.036). No significant group or time effect was noted on the ADDQOL.
Discussion and conclusions: An integrated HF-DM self-care intervention was effective in improving essential components of self-care, including exercise and foot care behavior and perceived physical aspect of HF physical QOL. Improving overall self-care behaviors was associated with improved HF QOL. These relationships were not observed for the DM QOL and self-care variables. Future studies testing HF-DM integrated self-care interventions with longer follow up in a larger sample are warranted.
Proudly powered by Weebly