-
Butts Research
- Meet the Team
- Metabolomic Pathways of Symptoms in Black Adults with Heart Failure
- Skeletal Muscle in Heart Failure with Preserved Ejection Fraction
- Inflammasome in Heart Failure
- Exercise and Heart Failure
- Telomeres in Heart Failure
- Heart Failure Research Studies
- Publications
- Presentation Abstracts
- Atlanta Heart Failure Knowledge Test
- PREVAIL Lab
- MVP Study
- CARDI Study
- Past Studies
- Health Information
- Pathophysiology Videos
- Genetics Workshop (UNC)
- Omics Workshop (SNRS 2023)
- AHFKT
You can download a copy of the AARP Georgia Diabetes Prevention and Insulin Education presentation here.
Additional links and resources
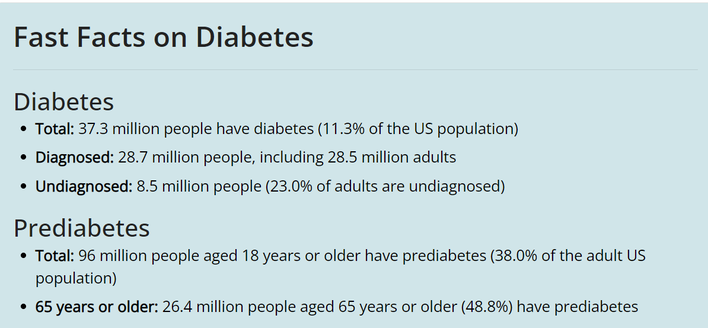
Diabetes in the United States
The US Centers for Disease Control and Prevention (CDC) tracks the number of people living with diabetes (prevalence) and the number of people newly diagnosed with diabetes each year (incidence). You can find more information on the CDC website: https://www.cdc.gov/diabetes/data/statistics-report/index.html
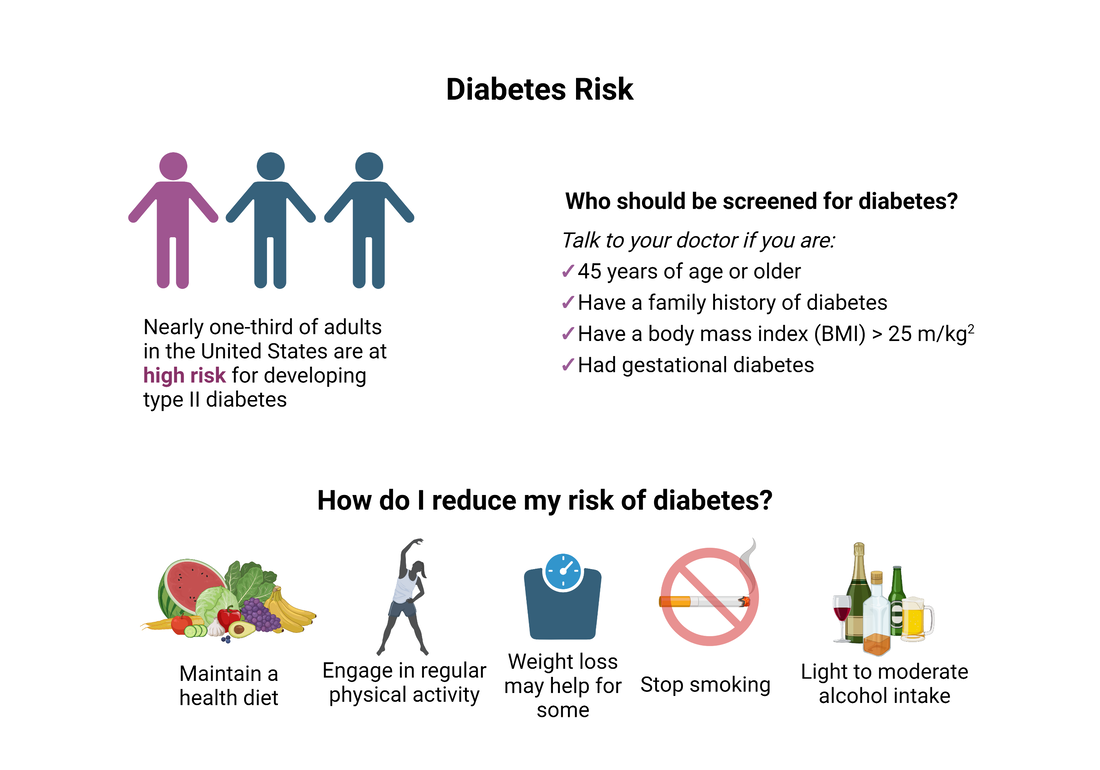
What are the risk factors for diabetes?
Risk factors for diabetes vary by individual. You can learn more about diabetes risk factors here: https://www.cdc.gov/diabetes/basics/risk-factors.html
Or check out this diabetes prevention guide!
For type I diabetes, having a relative with type I diabetes is the biggest risk factor.
For type II diabetes, risk factors include age, family history, and physical inactivity.
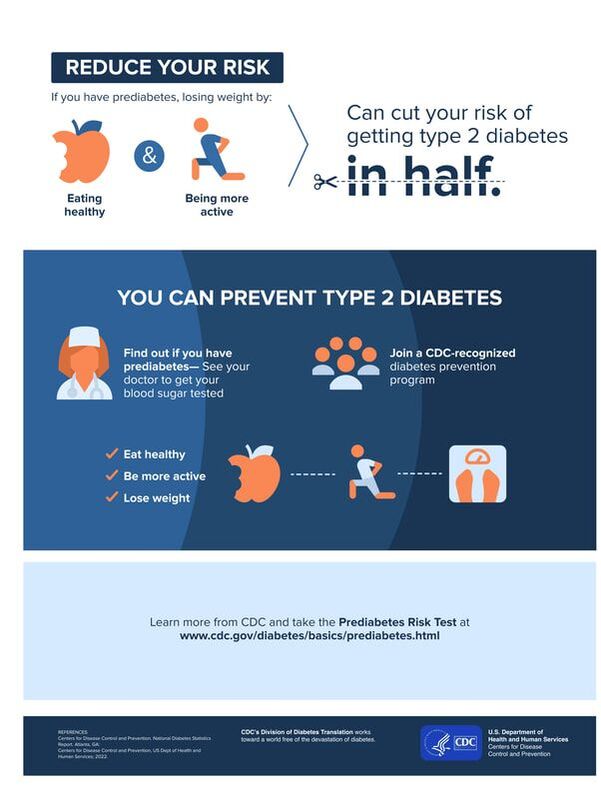
If you are interested in reducing your risk for developing type II diabetes, the CDC's Diabetes Prevention Program is a great place to start: www.cdc.gov/diabetes/prevention/index.html
Diabetes risk factor prevention strategies may include:
1. For some, a 7-10% reduction in weight can significantly reduce diabetes risk.
2. Increasing physical activity. Adults need 150 minutes of moderate-intensity physical activity and 2 days of muscle strengthening activity each week. This doesn't need to happen all at once! It could be 30 minutes a day, 5 days a week. You can spread your activity out during the week and break it up into smaller chunks of time. Even 10 minutes 3 times a day is a great way to meet your activity goals! Need tips to get started? Check out these tips: https://www.cdc.gov/healthyweight/physical_activity/getting_started.html
3. Adopt a diet full of fruits and vegetables, healthy grains, and healthy fats. Here are the key dietary goals for diabetes prevention:
4. For those that drink alcohol, light to moderate alcohol consumption is key.
5. Don't smoke. Smokers are roughly 50% more likely to develop diabetes than nonsmokers, and heavy smokers have an even higher risk.
Or check out this diabetes prevention guide!
For type I diabetes, having a relative with type I diabetes is the biggest risk factor.
For type II diabetes, risk factors include age, family history, and physical inactivity.
If you are interested in reducing your risk for developing type II diabetes, the CDC's Diabetes Prevention Program is a great place to start: www.cdc.gov/diabetes/prevention/index.html
Diabetes risk factor prevention strategies may include:
1. For some, a 7-10% reduction in weight can significantly reduce diabetes risk.
2. Increasing physical activity. Adults need 150 minutes of moderate-intensity physical activity and 2 days of muscle strengthening activity each week. This doesn't need to happen all at once! It could be 30 minutes a day, 5 days a week. You can spread your activity out during the week and break it up into smaller chunks of time. Even 10 minutes 3 times a day is a great way to meet your activity goals! Need tips to get started? Check out these tips: https://www.cdc.gov/healthyweight/physical_activity/getting_started.html
3. Adopt a diet full of fruits and vegetables, healthy grains, and healthy fats. Here are the key dietary goals for diabetes prevention:
- Include lots of fruit and vegetables to your diet.
- Choose whole grains and whole grain products over refined grains and other highly processed carbohydrates.
- Skip the sugary drinks, and choose water, coffee, or tea instead.
- Choose health fats, such as the polyunsaturated fats found in liquid vegetable oils, nuts, and seeds can help ward off type 2 diabetes.
- Limit red meat and avoid processed meat; choose nuts, beans, whole grains, poultry, or fish instead.
4. For those that drink alcohol, light to moderate alcohol consumption is key.
5. Don't smoke. Smokers are roughly 50% more likely to develop diabetes than nonsmokers, and heavy smokers have an even higher risk.
What is diabetes?
Diabetes is a chronic disease that affects how your body uses fuel. Diabetes is a disorder of carbohydrate, protein, and fat metabolism resulting from a lack of insulin availability or reduction in biologic effects of insulin. You can learn more about diabetes here: www.cdc.gov/diabetes/basics/diabetes.html
There are three types of diabetes:
1. Type I diabetes. People living with type I diabetes are unable to make any insulin. Type I diabetes is thought to be caused by an autoimmune disease, where the immune system destroys the cells that make insulin. People with type I diabetes must take insulin throughout their entire lives. Approximately 5-10% of people living with diabetes have type I diabetes.
2. Type II diabetes. People living with type II diabetes are able to make insulin. However, their bodies are unable to use the insulin very well. This is called insulin resistance. Over time, people living with type II diabetes may make too little insulin, which could require them to require insulin for their treatment. Approximately 90-95% of persons living with diabetes have type II diabetes.
3. Gestational diabetes. Gestational diabetes occurs when there are abnormalities of glucose regulation that first presents during pregnancy. Gestational diabetes increases the risk for the development of type II diabetes later.
There are three types of diabetes:
1. Type I diabetes. People living with type I diabetes are unable to make any insulin. Type I diabetes is thought to be caused by an autoimmune disease, where the immune system destroys the cells that make insulin. People with type I diabetes must take insulin throughout their entire lives. Approximately 5-10% of people living with diabetes have type I diabetes.
2. Type II diabetes. People living with type II diabetes are able to make insulin. However, their bodies are unable to use the insulin very well. This is called insulin resistance. Over time, people living with type II diabetes may make too little insulin, which could require them to require insulin for their treatment. Approximately 90-95% of persons living with diabetes have type II diabetes.
3. Gestational diabetes. Gestational diabetes occurs when there are abnormalities of glucose regulation that first presents during pregnancy. Gestational diabetes increases the risk for the development of type II diabetes later.
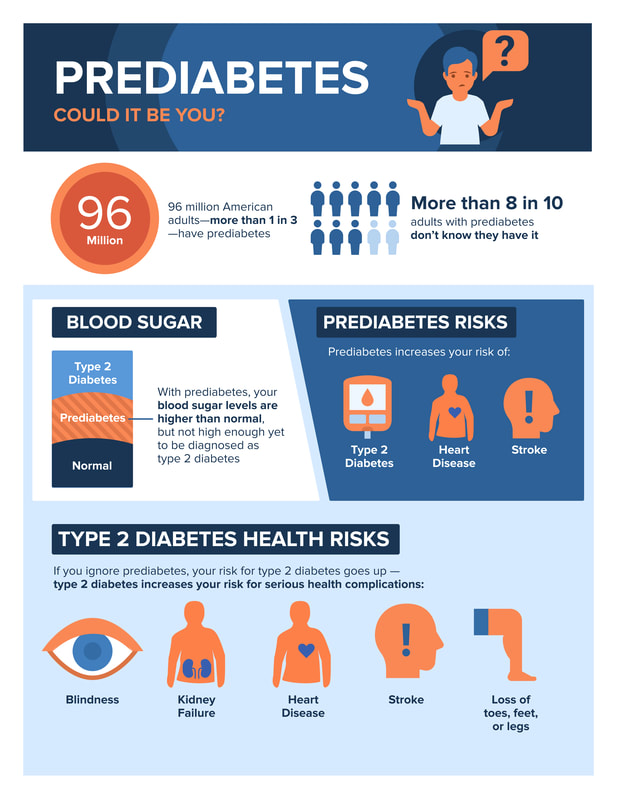
What is prediabetes?
Prediabetes is a condition where blood glucose (sugar) levels are higher than normal, but not high enough yet to be diagnosed as type 2 diabetes.
An estimated 96 million adults in the United States have prediabetes. Many people - more than 80% - are living with prediabetes and do not know they have it.
Prediabetes puts you at increased risk of developing type 2 diabetes, heart disease, and stroke. You should speak with your health care provider if you have any of the risk factors for diabetes and would like to be tested. If you do have prediabetes, the preventive lifestyle measures listed above can help lower your risk of developing type II diabetes.
You can learn more here: https://www.cdc.gov/diabetes/library/socialmedia/infographics/prediabetes.html
An estimated 96 million adults in the United States have prediabetes. Many people - more than 80% - are living with prediabetes and do not know they have it.
Prediabetes puts you at increased risk of developing type 2 diabetes, heart disease, and stroke. You should speak with your health care provider if you have any of the risk factors for diabetes and would like to be tested. If you do have prediabetes, the preventive lifestyle measures listed above can help lower your risk of developing type II diabetes.
You can learn more here: https://www.cdc.gov/diabetes/library/socialmedia/infographics/prediabetes.html
How is diabetes diagnosed?
There are several tests of your blood that may be done to check for diabetes. These tests all relate to your body's ability to remove glucose from the blood.
Plasma fasting glucose test – at least 8 hours with no caloric intake
Random blood glucose test – without regard to last meal
Oral glucose tolerance test (OGTT) – measures body’s ability to remove glucose from the blood.
This measures blood glucose before and after drinking a liquid that contains glucose. You will need to fast overnight before the test. Fasting blood sugar level is tested. After drinking the glucose solution (75g normally), blood sugar levels are checked 1 hour, 2 hours, and possibly 3 hours afterward. Blood glucose levels should return to normal within 2-3 hours.
Glycated hemoglobin (HbA1C) testing – measures quantity of glycated hemoglobin (glucose molecules on hemoglobin). This measures blood glucose levels over ~120-day lifespan of RBCs. When RBCs are first released from the bone marrow, hemoglobin normally does not contain glucose. During the lifespan of the RBC, hemoglobin normally becomes glycated. Because RBCs do not require insulin for glucose uptake, the rate at which glucose becomes attached to hemoglobin (glycosylation) reflects blood glucose levels. Glycosylation is generally an irreversible process.
Plasma fasting glucose test – at least 8 hours with no caloric intake
- Normal: below 100 mg/dL is normal
- Prediabetes: 100-125 mg/dL
- Diabetes: 126 mg/dL or above
Random blood glucose test – without regard to last meal
- Diabetes: 200 mg/dL or above
Oral glucose tolerance test (OGTT) – measures body’s ability to remove glucose from the blood.
This measures blood glucose before and after drinking a liquid that contains glucose. You will need to fast overnight before the test. Fasting blood sugar level is tested. After drinking the glucose solution (75g normally), blood sugar levels are checked 1 hour, 2 hours, and possibly 3 hours afterward. Blood glucose levels should return to normal within 2-3 hours.
- Normal: 140 mg/dL or below.
- Prediabetes: 140-199 mg/dL
- Diabetes: 200 mg/dL or above
Glycated hemoglobin (HbA1C) testing – measures quantity of glycated hemoglobin (glucose molecules on hemoglobin). This measures blood glucose levels over ~120-day lifespan of RBCs. When RBCs are first released from the bone marrow, hemoglobin normally does not contain glucose. During the lifespan of the RBC, hemoglobin normally becomes glycated. Because RBCs do not require insulin for glucose uptake, the rate at which glucose becomes attached to hemoglobin (glycosylation) reflects blood glucose levels. Glycosylation is generally an irreversible process.
- Normal: below 5.7%
- Prediabetes: 5.7-6.4%
- Diabetes: 6.5% or above
What is insulin?
Insulin is a hormone made by our pancreas, a small organ behind our liver. Insulin is required to move glucose (the sugar in our blood) out of the blood and into our cells. Our cells need glucose for energy. You can read more about insulin here: https://www.cdc.gov/diabetes/basics/insulin-resistance.html
In persons living with diabetes, individuals may not make any insulin or may have trouble with their body using insulin (insulin resistance).
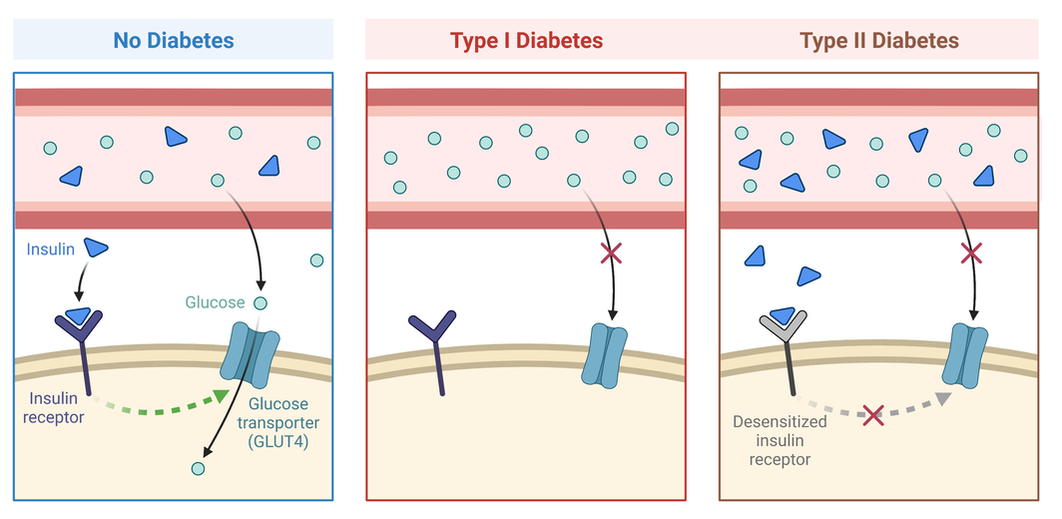
The sugar in our blood (glucose) cannot enter the cell on its own. It needs to go through a special gate that only insulin can unlock. So, insulin is the key we need to unlock the glucose gate.
In type I diabetes, there is no key to open the gate. These individuals need to take insulin as a medication to get that key into their system and unlock the glucose gate.
In type II diabetes, the key has trouble fitting into the lock on the glucose gate, so they can only open that gate sometimes. But it isn't enough. Individuals living with type II diabetes will take medications that help regulate their blood sugar. This treatment may or may not include insulin. (Please see below for types of diabetes medications.)
In persons living with diabetes, individuals may not make any insulin or may have trouble with their body using insulin (insulin resistance).
The sugar in our blood (glucose) cannot enter the cell on its own. It needs to go through a special gate that only insulin can unlock. So, insulin is the key we need to unlock the glucose gate.
In type I diabetes, there is no key to open the gate. These individuals need to take insulin as a medication to get that key into their system and unlock the glucose gate.
In type II diabetes, the key has trouble fitting into the lock on the glucose gate, so they can only open that gate sometimes. But it isn't enough. Individuals living with type II diabetes will take medications that help regulate their blood sugar. This treatment may or may not include insulin. (Please see below for types of diabetes medications.)
In this picture, you can see that insulin, represented by the blue triangles, are the key that unlocks the glucose gate. In the individual without diabetes, the insulin circulating in the blood unlocks the glucose gate, allowing glucose to move into the cell. In the individual with type I diabetes, there is no insulin in the blood, so there is no key to unlock the glucose gate. Glucose stays in the blood and is unable to move into the cell to provide energy to the body. In the individual with type II diabetes, there is insulin in the blood. However, the insulin key no longer unlocks the glucose gate all of the time, so much of the glucose stays in the blood.
What medications are used for diabetes?
There are different types of medications used for diabetes. Treatment for diabetes may or may not include insulin.
For persons living with type I diabetes, their treatment is insulin. There are different types of insulin, which are explained here:
There are three main groups of insulins, categorized based on onset (how quickly they act), peak (how long it takes to achieve maximum impact), and duration (how long they last before they wear off).
1. Fast-acting insulin
2. Intermediate-acting insulin
3. Long-acting insulin
There are also combined regular- or short-acting and intermediate-acting insulin, which include:
Persons with type II diabetes may take different types of medications. Some of the most common medications for persons with type II diabetes include:
It is important to remember that persons living with type II diabetes may also require insulin as part of their medication therapy.
For persons living with type I diabetes, their treatment is insulin. There are different types of insulin, which are explained here:
There are three main groups of insulins, categorized based on onset (how quickly they act), peak (how long it takes to achieve maximum impact), and duration (how long they last before they wear off).
1. Fast-acting insulin
- Absorbed quickly from your fat tissue (subcutaneous) into the bloodstream.
- Usually taken before a meal to control the blood sugar during meals and snacks and to correct high blood sugars
- Includes rapid acting and regular/short acting.
- Rapid-acting insulin include: insulin aspart (NovoLog), insulin glulisine (Apidra), and insulin lispro (Humalog)
- Regular- or short-acting products generally use insulin regular include: Humulin R, Humulin R U-500, Humulin R U-500 KwikPen, Novolin R, Novolin R Innolet, Novolin R PenFill, ReliOn/Humulin R, and ReliOn/Novolin R
2. Intermediate-acting insulin
- Absorbed more slowly, and lasts longer.
- Used to control the blood sugar overnight, while fasting and between meals.
- Intermediate-acting products generally use insulin isophane, including: Humulin N Humulin N KwikPen, Humulin N Pen, Novolin N, Novolin N Innolet, Novolin N PenFill, and ReliOn/Novolin N
3. Long-acting insulin
- Absorbed slowly, has a minimal peak effect, and a stable plateau effect that lasts most of the day.
- Used to control the blood sugar overnight, while fasting and between meals.
- Long-acting insulin products include:
- Insulin detemir (Levemir, Levemir FlexPen, Levemir FlexTouch, Levemir InnoLet, Levemir PenFill)
- Insulin degludec (Tresiba FlexTouch)
- Insulin glargine (Basaglar KwikPen, Lantus, Lantus OptiClik Cartridge, Lantus Solostar Pen, Toujeo Max Solostar, Toujeo SoloStar)
There are also combined regular- or short-acting and intermediate-acting insulin, which include:
- Blends of insulin isophane and insulin regular (Humalin 50/50, Humulin 70/30, Humulin 70/30 KwikPen, Novolin 70/30, ReliON/Novolin 70/30)
- Blends of insulin lispro and insulin lispro protamine (Humalog Mix 75/25, Humalog Mix 75/25 KwikPen)
Persons with type II diabetes may take different types of medications. Some of the most common medications for persons with type II diabetes include:
- Metformin
- DPP-4 inhibitors
- GLP-1 and dual GLP-1/GIP receptor agonists
- SGLT2 Inhibitors
- Sulfonylureas
- Thiazolidinediones (TZDs)
It is important to remember that persons living with type II diabetes may also require insulin as part of their medication therapy.
What are the complications of diabetes?
There are short-term (emergency) and long-term (chronic) complications that can occur in persons living with diabetes.
Emergency complications include:
Chronic complications include:
Diseases of the small blood vessels in the body:
Emergency complications include:
- Hypoglycemia occurs when the the blood sugar is too low.
- Diabetic ketoacidosis (DKA) occurs when the blood sugar is too high.
- Hyperosmolar hyperglycemic state (HHS) occurs in persons with type II diabetes with very high blood sugar.
Chronic complications include:
Diseases of the small blood vessels in the body:
- Diabetic retinopathy, which causes visual changes or vision loss.
- Diabetic nephropathy, which causes kidney disease or kidney failure
- Diabetic neuropathies, which causes problems with nerves, such as numbness or tingling.
- High blood pressure
- Heart disease and heart attack
- Heart failure
- Stroke
- Peripheral vascular disease
- Wound infections that do not heal
- Foot ulcers
Proudly powered by Weebly